Urinary Incontinence
What is Urinary Incontinence?
Urinary incontinence is a loss of bladder control that causes urine leakage and affects up to 50 percent of women at some point in their lives. Although the risk for urinary incontinence increases with age, many young women also suffer from these symptoms. If you find yourself avoiding exercising or socializing because you’re worried about “leaks” or accidents, our experts can help.
Even though urinary incontinence is common, it is not normal at any age. Yet there’s no need to be ashamed to talk to a specialist about your symptoms. The urogynecologists at the University of Chicago Medicine are experts in treating urinary incontinence and have helped others like you put an end to their distressing symptoms. The sooner you seek treatment, the sooner you can find relief.
Depending on the type of urinary incontinence you experience, your symptoms can be successfully treated using non-surgical therapies (such as physical therapy, medication or pessaries) or simple outpatient non-invasive procedures (slings, pacemakers or urethral bulking) to restore your quality of life.
Types of Urinary Incontinence
Stress Urinary Incontinence
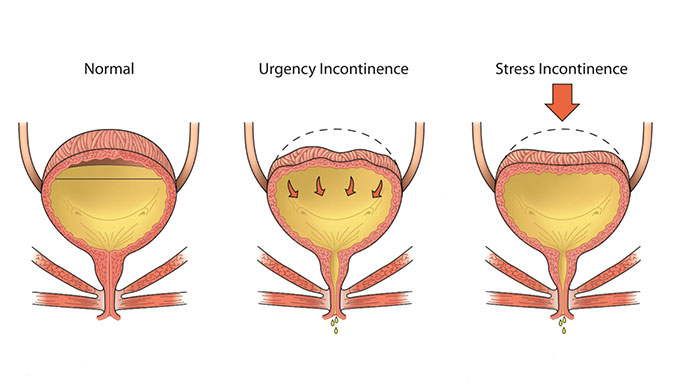
Leaking urine when you cough, sneeze or exercise is a symptom of stress urinary incontinence, the most common type of urinary incontinence. It occurs in nearly one-third of young women after delivering a baby, and it is even more common as we get older and after menopause. Stress incontinence is a result of damage to nerves and muscles that are meant to keep the urethra closed during activities that increase abdominal pressure. When the urethra stays open, this allows urine to leak out with increases in abdominal pressure.
Treatment for Stress Urinary Incontinence
Urgency Urinary Incontinence (Overactive Bladder)
This type of urinary leakage is often associated with frequent urination (more than eight voids in a day) and urinary urgency or a strong sensation of the need to urinate. Women often report waking up to go to the bathroom in the middle of the night and/or rushing to go to the bathroom but not making it in time. In urgency urinary incontinence, the bladder squeezes or contracts before it is full because it is “overactive” or the nerve signals between your brain and bladder don’t work properly.
Treatment for Urgency Urinary Incontinence
Mixed Urinary Incontinence
This type of incontinence is common and is a combination of stress and urgency urinary incontinence.
Functional Urinary Incontinence
This type of urinary leakage occurs in patients whose bladder and urethra (the tube that allows urine to exit your body) work normally, but they have a physical or medical condition that limits their ability to get to the restroom in time.
Overflow Urinary Incontinence
This type of urinary leakage occurs in patients who do not completely empty their bladder, so it stores excess urine and some “leaks” out.
Frequently Asked Questions about Urinary Incontinence
Symptoms will vary depending on the type of urinary incontinence, but all women with urinary incontinence experience accidental leaking of urine. For example, if you have stress urinary incontinence, you leak urine when you cough, sneeze, laugh or do physical activity like running and cycling. Or if you have urgency urinary incontinence, you will have frequent and strong senses of urinary urgency and you might not feel like you can make it to the bathroom in time, sometimes resulting in leakage episodes.
Such symptoms bother some women more than others. While it is not normal to leak urine, if your symptoms do not bother you, you do not need to seek treatment. But if they do disturb you, don’t hesitate to talk with one of our experts, who can suggest treatment options.
At your visit, your urogynecologist will review your concerns and treatment preferences and ask additional questions about your symptoms and which activities or situations cause you to leak urine. Your urogynecologist may also perform a physical exam and take a urine sample. You may also be asked to complete a urinary diary, which means recording how much you drink and urinate.
Your urogynecologist may also order additional tests to determine the type of urinary incontinence you have.
To help diagnose urinary incontinence, your urogynecologist may order tests, including:
- Cough stress test to determine if you leak urine from the urethra with increases in abdominal pressure
- Urodynamic testing to learn how your bladder and urethra work as your bladder fills and empties
- 3D pelvic ultrasound to examine your pelvic floor and anal sphincter muscles
- Cystoscopy to look inside your bladder and urethra with a small tube attached to a camera
- Post-void residual urine test to make sure you empty your bladder completely
At UChicago Medicine, your urogynecologist will develop an individualized care plan to address your symptoms and personal goals for treatment. We offer nonsurgical treatments as well as minimally invasive, outpatient surgical options and will work with you to determine the best approach. This may include a combination of treatments to help relieve your symptoms. Your treatment will be tailored to your individual needs after meeting with your urogynecology team.
Meet Our Urogynecologists

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery
