Urgency Urinary Incontinence (Overactive Bladder)
If you have urgency urinary incontinence, also known as overactive bladder, you may have the following symptoms:
- Urinating frequently (more than eight times a day)
- Feeling a strong need to urinate
- Rushing to the bathroom and leaking urine
- Waking up at night to urinate
These symptoms can occur when the nerve signals between your brain and bladder no longer work properly. This can cause your bladder to squeeze, or contract, before it is full.
Urgency Urinary Incontinence/Overactive Bladder Treatments
Most treatments for urgency urinary incontinence aim to decrease abnormal bladder contractions that cause urinary leakage.
Your urogynecologist will work with you to determine the best approach — which may include one or more treatment options — to relieve your symptoms and support your health goals.
Lifestyle Changes
Lifestyle changes can improve or lessen symptoms of urgency urinary incontinence. It may help if you:
- Limit caffeine, alcohol and sugary drinks, which cause you to urinate more frequently
- Go to the bathroom more frequently (every two to three hours)
- Increase the amount of fiber in your diet to treat constipation, which can make you feel like you need to urinate
- Stop smoking, which doubles your risk for developing a pelvic floor disorder
- Maintain a healthy weight or lose weight if you are overweight
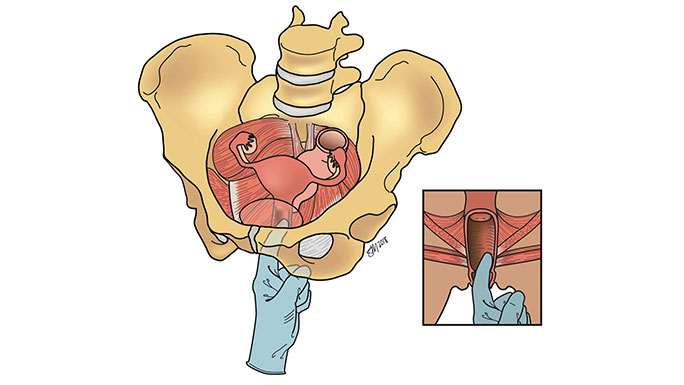
Pelvic Floor Physical Therapy
Pelvic floor physical therapy helps restore proper function of your pelvic floor muscles. If you and your urogynecologist decide that pelvic floor physical therapy is the right treatment option for you, they will provide you with a referral to a pelvic floor physical therapist.
Medication
Medications can reduce symptoms of urgency urinary incontinence, although they have different success rates and side effects. Your urogynecology team will help determine if these are good options for you. Some options include:
- Local vaginal estrogen, in the form of a low-dose estrogen cream or tablet placed in the vagina, can improve symptoms of urinary frequency, urgency and urgency urinary incontinence by replenishing vaginal and urethral tissues.
- Antimuscarinic oral medications taken once a day can treat urgency urinary incontinence. Some examples include solifenacin, fesoterodine, tolterodine, darifenacin, trospium and oxybutynin. Although they are effective at treating urgency urinary incontinence, these medications often cause bothersome side effects, such as dry mouth and constipation. New research has also found that persistent use of these medications is associated with memory changes or dementia.
- Beta-3 agonist oral medications, such as mirabegron, can also be taken once a day to relax the bladder muscle and decrease unwanted contractions that cause urine leakage. These medications may be safer than antimuscarinic medications when taken over many months or years and are not associated with memory changes or dementia.
Treatment Procedures for Urgency Urinary Incontinence
Many women choose to have procedures for urgency urinary incontinence instead of, or in combination with, lifestyle treatments and medications.
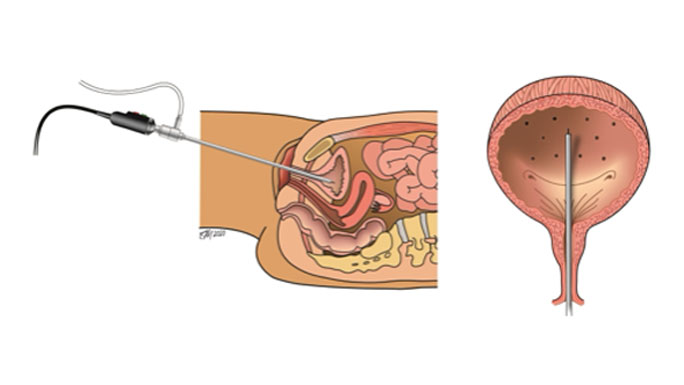
At UChicago Medicine, our urogynecologic surgeons offer several highly effective, noninvasive treatments that can be performed in the office or at an outpatient surgical center with few risks and minimal downtime. They include:
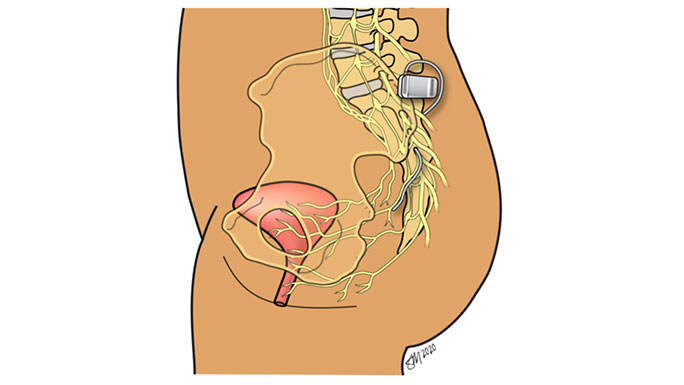
Sacral neuromodulation is a minimally invasive procedure that effectively treats urgency urinary incontinence, urgency/frequency, urinary retention and anal incontinence by providing gentle stimulation to the nerves that control the bladder and bowel.
Meet Our Urogynecologists

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery

Urogynecology and Reconstructive Pelvic Surgery
