HPV-Related Head and Neck Cancer Treatment
Request an Appointment
We are currently experiencing a high volume of inquiries, leading to delayed response times. For faster assistance, please call 1-855-702-8222 to schedule your appointment.
If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
For Referring Physicians
To refer a patient for head and neck cancer care, please call UCM Physician Connect at 1-800-824-2282.
* Indicates required field

Cancer Care Second Opinions
Request a second opinion from UChicago Medicine experts in head and neck cancer care.

Participate in a Clinical Trial
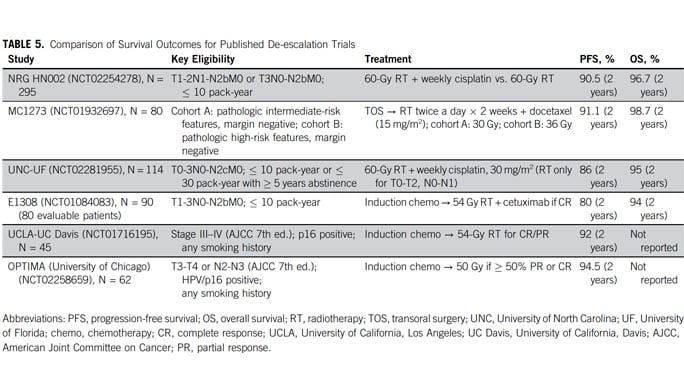
UChicago Medicine head & neck cancer experts are actively conducting clinical trials of new and promising treatments.

Helping You Cope With Cancer
Our Supportive Oncology program offers a range of services to support you and your family during your cancer treatment.
Head & Neck Cancer: Q & A

Head & Neck Cancer: Q & A
Medical oncologist Alexander T. Pearson, MD, PhD, and nurse navigator Patricia Heinlen, BSN, RN, discuss head and neck cancer, including the HPV vaccine and how new treatment approaches are tailored to each patient's cancer type, making treatments more effective while reducing side effects.