Gastroesophageal Reflux Disease (GERD)
The University of Chicago Medicine is home to one of the few centers in the United States that is dedicated to diagnosing and treating esophageal disorders, including gastrointestinal reflux disease (GERD) in adults and children. Our program allows our physicians to specialize in esophageal conditions and help patients with GERD on a daily basis.
Request an appointment for GERD
Providing the very best treatment options for patients is a key priority. We offer a full range of medical, surgical and minimally invasive treatment options to meet each patient’s needs, including minimally invasive GERD surgery that can provide lasting relief without the side effects of taking medications for decades. We continually evaluate the results of our treatment approaches and work to improve surgical and medical solutions for patients.
What is GERD?
Gastrointestinal reflux disease (GERD) is more than just heartburn. Untreated, GERD can develop into more serious conditions, including cancer for a small percentage of individuals.
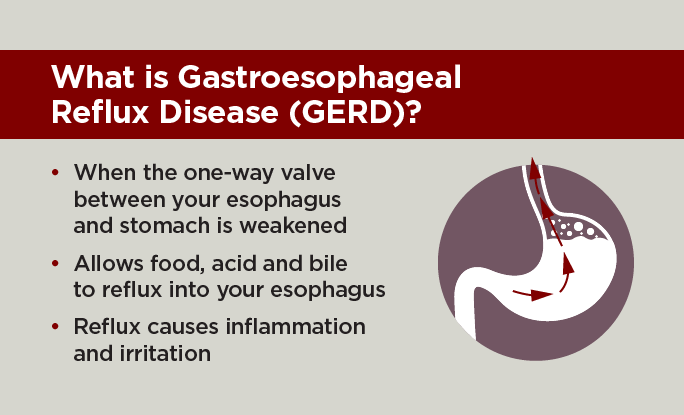
It’s normal to experience gastroesophageal reflux (also known as acid reflux) once in a while after eating. For most people, this acid reflux is a mild form of heartburn that can be controlled with over-the-counter medications, changes in food choices or changes in the quantity eaten at one time. If mild heartburn persists, your primary care doctor may prescribe a stronger medication. In comparison, gastroesophageal reflux disease (GERD) is less common but more troublesome than periodic acid reflux.
GERD can produce a broad variety of symptoms, including:
- Asthma
- Belching
- Bloating
- Chest pain
- Chronic cough
- Difficulty swallowing (dysphagia)
- Early satiety (feeling full after eating a little food)
- Excess saliva (water brash)
- Feeling of a lump in the throat (globus)
- Heartburn
- Hoarseness
- Lung aspiration
- Nausea
- Regurgitation
- Shortness of breath (dyspnea)
- Voice problems
- Wheezing
People with cystic fibrosis are more likely to experience GERD symptoms than the average person.
A one-way valve — called the lower esophageal sphincter (LES) — allows food to pass into your stomach and prevents stomach acid from flowing back up into the esophagus. When this valve is weakened and not functioning properly, gastric juice comes up from the stomach and back into the esophagus causing irritation and inflammation (esophagitis). Over time, this can damage to the lining of the esophagus. Nearly half of patients with GERD will develop esophagitis, and up to 15 percent of patients with GERD may develop a pre-cancerous condition called Barrett’s esophagus. A small percentage of people with Barrett’s esophagus will progress to esophageal adenocarcinoma — a form of cancer in the esophagus. A second type of esophageal cancer — squamous cell carcinoma — is not related to GERD or Barrett’s esophagus.
GERD can lead to more serious conditions if not diagnosed and treated properly. If you have experienced GERD for a number of years, it is important to have your esophagus checked for changes.
Proper diagnosis is the first step toward effective treatment. Depending on their unique symptoms, patients may turn to different types of physicians for solutions, such as gastroenterologists, otolaryngologists, cardiologists or pulmonologists. UChicago Medicine's Center for Esophageal Diseases draws together specialists from all of these areas to collaborate as needed.
Doctors may recommend some or all of the following tests to pinpoint the cause of symptoms:
- Ambulatory impedance-pH monitoring: This test measures the frequency and amount of gastric contents (acid and non-acid) that refluxes from the stomach to the esophagus, usually over a 24-hour period. This test involves threading a very thin tube (catheter) through the nose and down the esophagus. The catheter is attached to a monitoring system. “Ambulatory” means that you can walk around and do your normal activities while wearing this monitor.
- Endoscopy: A thin, flexible tube equipped with a tiny camera and light is inserted through the mouth and down the throat. Diagnostic endoscopy enables the physician to see inside the throat and into the stomach.
- Esophageal motility testing: Our state-of-the-art esophageal motility lab has advanced technology to evaluate how well the muscles of the esophagus are functioning. Specifically, testing provides information about the function of the valve located between the esophagus and the stomach and the ability of the esophageal muscles to squeeze.
- X-ray: Involving a barium swallow to see if there is a hiatal hernia or a stricture of the esophagus.
In most cases, GERD is a chronic condition that people live with for the rest of their lives. The only curative treatment is surgery, but medications and lifestyle changes are helpful for managing the symptoms of GERD. Our physicians and surgeons can help patients decide which treatment option best fits their needs.
For most patients, treatment recommendations follow a stepped approach that begins with changes in diet, avoiding food close to bedtime, losing weight and reducing and eliminating smoking and alcohol use.
Medical Treatment
When lifestyle changes do not work, medications designed to suppress the production of excess acid are typically the next step. Antacids or histamine H2 receptor agonists therapy can be effective for many individuals with mild to moderate symptoms. Additional H2 blocker therapy or proton pump inhibitor medications may be prescribed for symptoms that are more persistent. Medications, however, are less effective when a large hiatal hernia, regurgitation, aspiration, cough and/or voice problems are present. While medications can lessen or control the symptoms of GERD, they do not cure this chronic disorder. Therefore, patients take the medications for the rest of their lives or as symptoms dictate.
Surgical Treatment
A number of patients with GERD may be appropriate candidates for surgical treatment with an anti-reflux procedure. This procedure tightens the valve located between the stomach and the esophagus, called the lower esophageal sphincter, which prevents the stomach contents and acid from refluxing back into the esophagus. Unlike medications that provide only symptomatic heartburn relief, anti-reflux surgery can stop GERD symptoms for most patients, including regurgitation, trouble swallowing and voice changes.
If you have GERD, you have a higher risk for Barrett’s esophagus. People with this condition can develop a rare type of esophageal cancer. Although the overall risk for esophageal cancer is extremely low, we recommend getting a screening test called a surveillance esophagogastroduodenoscopy (EGD) every three to five years if you have GERD.
During an EGD, a doctor uses a thin tube, or endoscope, with a camera to check for changes inside of your esophagus.
If you have GERD and your symptoms still bother you even though you take medication, you may be a candidate for surgery.
Even if your symptoms are controlled with medication, you may want to see a gastrointestinal surgeon so you can understand your options. Surgery may provide better control of your symptoms and reduce your need for medication.
Several procedures are available to help reduce GERD symptoms, from fundoplication to weight loss surgery, if needed. At UChicago Medicine, we’ll work with you to determine the best option so that you can find relief from your symptoms.
Surgery can be offered to all patients with GERD, but should be strongly considered for:
- Patients that do not experience relief of symptoms with medications
- Patients with voice or respiratory problems, including hoarseness, cough or asthma due to reflux
- Patients with a hiatal or paraesophageal hernia, making it difficult to eat
- Young patients, to avoid the cost and diminishing effectiveness of taking medications for many decades
- Patients with Barrett's esophagus
- Individuals with a BMI greater than 35
- Post-menopausal women, for whom some anti-GERD medications raise the risk of osteoporosis
Our surgeons use the latest techniques in robotic surgery and can perform many procedures using “hidden” incisions, so small scars are concealed below the waistline.
Each surgery we perform is personalized to the needs of each patient. For example, our surgeons use special technology called impedance planimetry during your GERD surgery to customize your procedure. This allows surgeons to measure the pressure and movement inside your esophagus and the connection to your stomach in real time so they can tailor your surgery based on your specific anatomy.
Anti-Reflux Treatment Options for GERD
Anti-reflux surgery is very effective for treating gastroesophageal reflux disease. The different anti-reflux operations described below are performed by specialized esophageal surgeons at UChicago Medicine through small incisions using minimally invasive techniques. These procedures all work by recreating the damaged valve between the esophagus and stomach.
Minimally Invasive GERD Surgery
Our expert surgeons at UChicago Medicine with specialized training in minimally invasive techniques use high definition laparoscopy and advanced robotic technology, making anti-reflux surgery a very safe and effective treatment option. These operations are performed using small, less than ½ inch cuts in the skin. This allows for not only less scaring, but also faster and easier recovery and less pain for patients. Using these minimally invasive techniques most patients go home later that day or the next day.
Which GERD surgery is best for me?
Our surgeons understand that every patient is unique. Depending on each your personal goals after surgery, your comfort with the procedure and your overall health, our team will help you make the right choice for you.
The different types of GERD surgeries include:
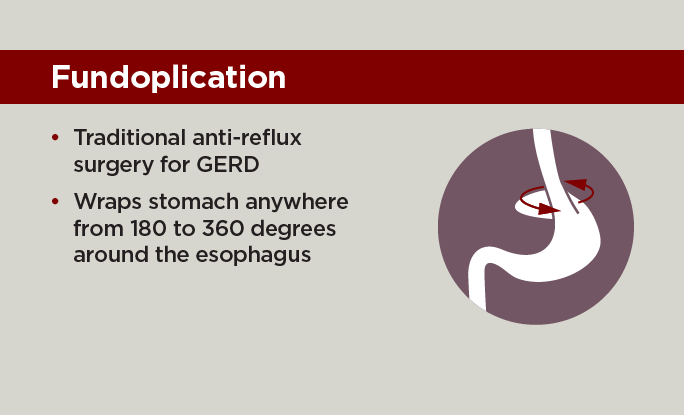
Fundoplication. Fundoplication has been the standard operation for GERD treatment for nearly 50 years. This operation involves a wrap of the stomach around the esophagus to reconstruct the lower esophageal sphincter to function as a one-way valve again.
This wrap of the stomach is called a fundoplication. A fundoplication can be a full 360-degree wrap or a partial wrap ranging from 180 to 270 degree, which allows for the best reconstruction of the valve to control reflux.
The degree of wrapping varies based on the patient and their valve function. We use special techniques to customize this wrap to the patient to prevent the valve from being too tight, but still controlling reflux symptoms.
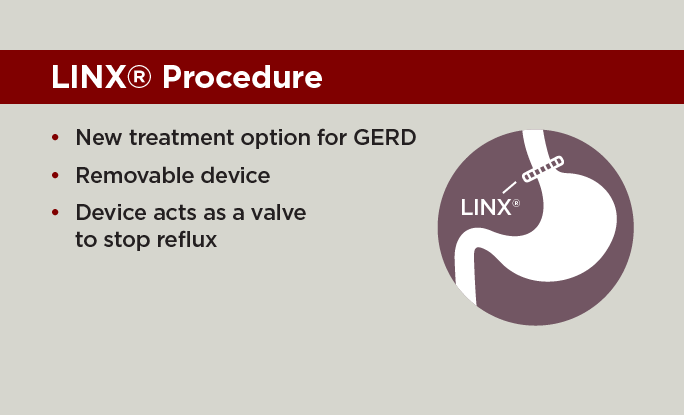
LINX Procedure. The LINX System is a new treatment option for patients with GERD. This removable device is a small, flexible ring of magnetic, titanium covered beads that acts as a valve to stop reflux from the stomach. The LINX system is designed to stay closed at rest to prevent acid reflux back into the esophagus, but then will expand with a normal swallowing mechanism to allow food and drink to pass into the stomach.
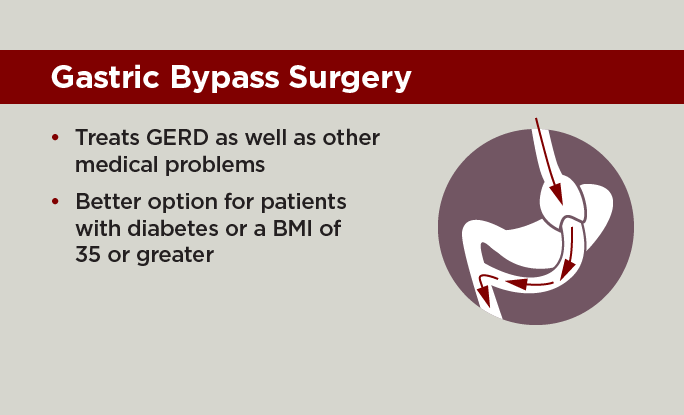
Gastric bypass surgery. Gastric bypass surgery may be an option in a select group of patients that have other medical conditions in addition to reflux. This operation works to treat reflux as well as diabetes, hypertension, sleep apnea, arthritis and allows for dramatic weight loss. Patients with a BMI 35 or higher may be a candidate for this treatment and can be discussed as a treatment option for you.
Transoral Incisionless Fundoplication (TIF). One of the latest options for GERD is called transoral incisionless fundoplication (TIF). This outpatient procedure may be used instead of traditional fundoplication in some patients.
During a TIF, a gastroenterologist inserts a long, thin tube called an endoscope with specially designed instruments down your esophagus to repair your valve without any incisions. Patients who have TIF often have a shorter recovery, compared with traditional fundoplication.

Nationally Ranked in Gastroenterology and GI Surgery
According to U.S. News & World Report's 2024-25 Rankings.
Learn more about U.S. News Best HospitalsTreating five medical problems with one surgery
Gastric bypass surgery was an option for Michael Meadows who had other medical conditions in addition to reflux. This operation works to treat reflux as well as chronic conditions, including diabetes, hypertension, sleep apnea, arthritis and allows for dramatic weight loss.

Request an Appointment
We are currently experiencing a high volume of inquiries, leading to delayed response times. For faster assistance, please call 1-888-824-0200 to schedule your appointment.
If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
You can also schedule an appointment instantly for in-person and video visits through our online scheduling portal.
* Indicates required field
