Stress vs. urgency incontinence: Understanding the types of bladder leakage

As a urogynecologist and reconstructive pelvic surgeon, I often encounter patients who think bladder leakage, otherwise known as urinary incontinence, becomes normal after a certain age. This is actually a misconception, and I want to help people understand more about their options when it comes to any leakage that happens outside of their control.
Is it normal to have bladder leakage?
Like diabetes or high blood pressure, bladder leakage is considered a disease. While it’s common, we don’t consider it a normal part of aging.
What are the types of urinary incontinence?
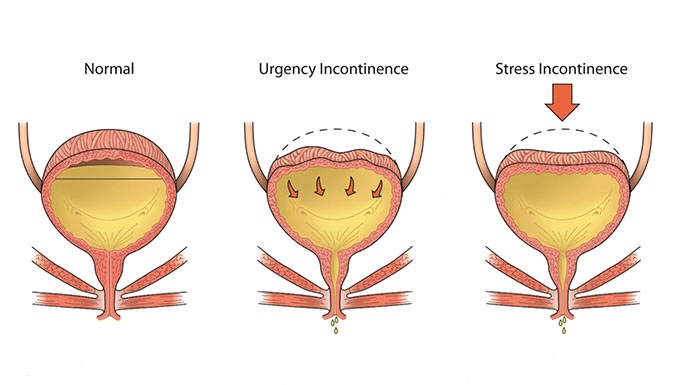
We tend to classify incontinence as either stress incontinence or urgency incontinence (also known as overactive bladder).
What is stress incontinence?
Stress incontinence happens when activities like coughing, laughing, sneezing or exercise put pressure on the bladder.
Who experiences stress incontinence?
About one-third of stress incontinence cases happen to women in their reproductive years. The other two-thirds are women ages 65 and older, though it can also happen to women following hysterectomies.
What causes stress incontinence?
Stress incontinence is caused by a problem with the urethral sphincter, which is the muscle that helps keep the urethra closed when the bladder or urethra experience pressure. People can have different risk factors for this, such as carrying a pregnancy with vaginal deliveries that weaken those muscles and cause the urethra to stay a little bit open. That neuromuscular decline can continue as women age.
What is overactive bladder/urgency incontinence?
Like the name implies, overactive bladder happens when someone has an overly frequent need to urinate, even if their bladder isn’t very full. This can become urgent and lead to leakage.
What causes urgency incontinence?
Aging is the predominant risk factor. As we age, sometimes our bladders stop responding as well to signals from our brain that are trying to indicate it’s not a socially appropriate time to go to the bathroom. Colloquially, we say the bladder develops a mind of its own. People in certain professions, like teaching or nursing, who have difficulty taking breaks from their jobs, do what we call “chronic postponing,” which can lead to an overactive bladder over time.
How can I prevent incontinence?
While C-sections aren’t an option for everyone, we know that avoiding vaginal deliveries eliminates one risk factor. There is some evidence showing that pelvic floor physical therapy immediately following deliveries can help prevent stress incontinence as we age. We also encourage everyone to avoid chronic postponing, if possible, and listen to your bladder when it’s telling you that you should go.
Are there other types of incontinence?
Mixed urinary incontinence, which is a combination of stress and urgency incontinence, is common in women. There is another type of incontinence called overflow incontinence, which is more common in men with enlarged prostates that don’t allow the bladder to empty effectively.
How do you treat incontinence?
My colleagues and I refer to ourselves as quality-of-life surgeons because our goal is to match patients with treatment options that align with their goals. At our Northbrook location, we are a fully functional, freestanding clinic with the ability to diagnose and treat either type of urinary incontinence, along with other pelvic floor disorders. We have a range of treatment options, from physical therapy or surgery, and will work with patients to personalize a plan that works for them. To schedule an appointment, call 773-795-8777.

Margaret Mueller, MD
Margaret (Maggie) Mueller, MD, FACOG, FACS, is an internationally recognized urogynecologist and reconstructive pelvic surgeon.
Learn more about Dr. Mueller
UChicago Medicine Northbrook
Our UChicago Medicine Northbrook location will offer urogynecology and pelvic reconstructive surgery, gynecology (specifically endometriosis and uterine fibroids) and gastroenterology (IBD, general gastroenterology and motility disorders), as well as infusion (non-chemotherapy) and blood draw lab services.
Learn more