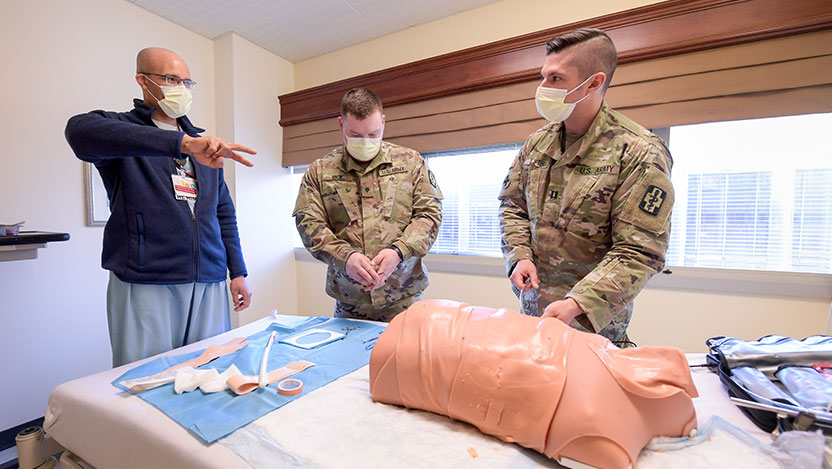
U.S. Army medical staff trains in UChicago Medicine’s Simulation Center

A new partnership between the U.S. Army and the University of Chicago Medicine brought 20 Army medics and advanced practice nurses to the hospital’s Simulation Center on April 9 to practice their emergency trauma skills.
The training sessions were led by four UChicago Medicine trauma doctors who also served in the military: Kenneth L. Wilson, MD, David Hampton, MD, Nicholas Jaszczak, MDTimothy Plackett, DO, MPH.
Using the Simulation Center’s lifelike, computer-controlled manikins, members of the 357th Army Reserve unit were able to practice treating war zone-like injuries with techniques such as intubations, applying tourniquets, suturing wounds, and using an ultrasound to assess gunshot or stab wounds.
Other hospitals may have simulation centers, but the level of training we provide separates us and makes us one of the leading places to train.
The Simulation Center’s manikins, which weigh as much as an adult human, are perfectly equipped for this. They can bleed, sweat, breathe, blink, moan and mimic unstable vital signs. Each also has a pulse and can be given an IV or a breathing tube. Computer software controls the manikin's response to treatment. For example, if a tourniquet isn’t placed correctly, the bleeding would not only continue but may spurt out of the wound.
The software also can change the manikin's physical characteristics to mimic clinical challenges. For example, the manikin's tongue can unexpectedly swell to prevent a breathing tube from going in easily, forcing the medic to make an adjustment.
“Other hospitals may have simulation centers, but the level of training we provide separates us and makes us one of the leading places to train,” said Robert Burgin, Assistant Director of the Simulation Center.
The training helps the Army medical staff maintain and sharpen their trauma care skills. Many currently work at local hospitals as reservists but lack experience with wartime injuries like gunshot wounds.
Army Lt. Sarah Van Wingerden, who works as a registered nurse in Austin, Texas, said this is the first time her group was able to work as a team in an “emergency” situation and it helped them learn each other’s skill sets and practice performing lifesaving procedures together.
“It’s been great. Today has been a great opportunity for our unit to get hands-on experience,” she said.

The Army medics, who arrived in their combat uniforms, also spent part of the day shadowing UChicago Medicine’s trauma doctors as they worked in the hospital’s emergency department, operating rooms and intensive care unit.
This marked the first time the U.S. Army has trained in UChicago Medicine’s Simulation Center, nicknamed the “Sim Center.” The center encompasses two wings of Mitchell Hospital plus a basement cadaver lab. It’s used by a wide range of groups, from high school students interested in healthcare careers to surgeons practicing minimally invasive surgery with the robotic da Vinci surgical system.
The Simulation Center recently changed leadership and is now led by Priti Jani, MD, a pediatric critical care specialist at Comer Children’s Hospital, Executive Director Melissa Cappaert and Burgin.
“It’s been great to establish this military and civilian relationship,” Cappaert said. “Our goal is to have an environment where people can practice their skills, so they’re prepared to provide the best care possible to their patients.”
The training is part of a program the U.S. Army launched in 2019 called AMCT3, which provides military medical teams an opportunity to practice their skills at busy hospital trauma centers across the country.
In 2021, now-retired UChicago Medicine President Sharon O’Keefe and Dean Kenneth Polonsky led the effort to have UChicago Medicine join the program, making it one of just seven AMCT3 training sites nationwide. Others include Vanderbilt University Medical Center in Tennessee, University of North Carolina Medical Center, Cooper University Hospital in New Jersey and Oregon Health & Science University Hospital.
You don’t want to learn how to shoot a layup in Game 7 of the NBA Finals. You need repeated practice so when the moment comes, you’re ready. This is such a great training for that.
As part of the program, Army medical personnel train in UChicago Medicine’s Emergency Department through embedded or short-term rotational assignments for up to three years. In 2021, a group of Army medics worked in the hospital’s Level 1 Trauma Center prior to their deployment.
The program also provides training for up to 30 Army medical personnel in the Simulation Center. They include Army surgeons, emergency medicine physicians, emergency and critical care nurses, anesthesiologists and certified nurse anesthetists, combat medics, operating room technicians, licensed practical nurses and other surgical subspecialties.
The partnership is mutually beneficial, Wilson said, since the military and civilian healthcare providers learn from each other and assist them in the busy ED. Wilson also hopes some of these talented, smart and disciplined military medics come to work at UChicago Medicine’s trauma center one day, like he did. Whether these skills save lives during a military operation or in a Chicago hospital, it benefits everyone.
“You don’t want to learn how to shoot a layup in Game 7 of the NBA Finals. You need repeated practice so when the moment comes, you’re ready. This is such a great training for that,” Wilson said. “We can simulate being immersed in a real trauma military environment.”
Follow UChicago Medicine’s Simulation Center on Twitter at @Simulation_uc
