Functional hemispherectomy stops seizures cold in kids with drug-resistant epilepsy

Joseph Riofski had his first seizure at age 4 ½.
Thus began a medical journey that led to admissions to two adult hospitals and three children’s hospitals, countless brain imaging and neurological tests, multiple intravenous immunoglobulin treatments, and trials of eight anti-seizure medications over the ensuing four years.
By the time Joseph was in second grade, he was having up to six seizures per day. He had to transfer to an elementary school where an assigned nurse stayed at his side to assist when he had a seizure during classes.
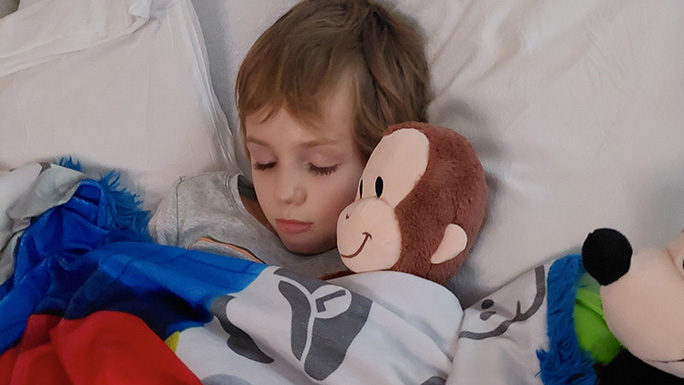
But mostly Joseph slept through his classes, the result of taking high doses of multiple anti-seizure medications. “Joseph was sleeping 18 hours per day, he wasn’t walking correctly, and he was stuttering,” said his mother, Sara Riofski. “Just walking from one room to another in our house could bring on a seizure, so I had to carry him everywhere and he was in a wheelchair at school.”
Despite numerous hospitalizations, neurologists couldn’t give the family a definitive diagnosis -- until Joseph was admitted to Comer Children’s Hospital.
“We suspected that Joseph had Rasmussen’s encephalitis,” said Douglas Nordli, Jr., MD, Chief of the Section of Pediatric Neurology and Co-Director of UChicago Medicine’s Comprehensive Epilepsy Center.
Meet our pediatric neurologists and neurosurgeons
Rasmussen’s encephalitis is a rare and disabling condition involving inflammation in one hemisphere of the brain. Believed to be autoimmune in nature, the disorder causes intractable seizures, profound weakness on the opposite side of the body, and neuropsychological issues such as deficits in working memory and brain processing speed.
Theodore Rasmussen, a neurosurgeon at the University of Chicago, first described the disorder in 1958. As a level 4 epilepsy center, UChicago Medicine epileptologists see pediatric patients with Rasmussen’s encephalitis fairly regularly. The disorder has an annual incidence of only 2.4 cases per 10 million children, said Nordli.
Anti-seizure medications may initially control the seizures, and some patients receive immune modulatory treatments to help arrest disease progression. But inevitably, the seizures become intractable, making a functional hemispherectomy the best option to arrest the seizures and restore patients’ quality of life.
Through a series of cuts in the brain, our expert pediatric neurosurgeons disconnect the diseased hemisphere from the contralateral hemisphere as well as all the diseased lobes from each other. The surgery functionally isolates the hemisphere impacted by severe epilepsy. This eliminates the need to remove large amounts of brain tissue, which can lead to a higher degree of complications.
For children with Rasmussen’s, early surgery offers the best chance of preserving brain function and reducing damage to the contralateral hemisphere from the abnormal electrical activity generated in the diseased hemisphere, said Nordli.
“The younger the child, the greater the plasticity in the brain, which allows some functions, such as language, to move to the contralateral hemisphere,” he said.
Other brain functions -- such as peripheral vision and fine finger movements -- are fixed, so a hemispherectomy won’t improve deficits in those areas.
But cognition generally improves after surgery. Patients typically do better cognitively because they're not having seizures throughout the day, enabling them to attend school and to learn.
Nordli recalled a patient whose IQ rose to 100, a normal intellect, from 80 before hemispherectomy. “The surgery freed her brain to function the way it was supposed to,” he said.
Despite the promise that their child will be seizure-free after hemispherectomy, parents often struggle with the decision to proceed with surgery when their child has residual neurologic function remaining in the diseased hemisphere. “It’s human nature to try to preserve every aspect of brain function in your child,” said Nordli.
Joseph’s parents were no exception. “We knew that hemispherectomy was the only way to help Joey, but it was so hard to convince ourselves that we were making the right decision because there was no going back and reattaching his brain if it didn’t work,” said Sara. “In the end, we wanted his seizures to end and for him to be a kid again.”
In July, our pediatric neurosurgeon performed a hemispherectomy on Joseph, a six-hour surgery. Today, 8-year-old Joseph is making remarkable strides, said his mother. Before surgery, Joseph was unable to participate in gym class or sports and frustrated that he was different than other kids. Today he exuberantly runs with his classmates on the playground, is seizure-free, and has discovered that he loves basketball.
Taking multiple anti-seizure medications had robbed Joseph of curiosity and interest in the world. “Now he asks constant questions, he understands and remembers the answers,” said Sara. “And he is smiling and laughing again. We owe our pediatric neurosurgeon the world because he gave us our son back. Joseph can now be a kid again.”
It requires a coordinated effort from a dedicated team of people, along with the right tools and expertise, to provide the state-of-the-art care worthy of a level 4 epilepsy center.
Four months after surgery, Joseph has limited functional movement in his left hand along with weakness on the left side of his body. With continuing physical therapy, some of Joseph’s motor function will improve over time.
Nordli recalled seeing a photo of Joseph wearing a backpack on the first day of school, only six weeks after his surgery. “Joseph’s brain had already moved many of the functions to the healthy hemisphere; it was a lovely thing to see,” said Nordli.
Joseph’s personality is back to what it was before he was having so many seizures. He’s doing great now, and he should continue to do well, our neurosurgeon explained.
Children with medically refractory epilepsy due to a stroke, hemimegalencephaly or Sturge-Weber syndrome are also candidates for functional hemispherectomy, provided one hemisphere is healthy. There are other neurosurgeries for refractory epilepsy, such as resection of a partial lobe or dysplastic tissue, or laser ablation.
Roughly 20% of children who develop epilepsy -- 53 per 100,000 children per year --will have intractable seizures, Nordli explained. Based on data from 20 years ago, only 27 per 1 million children each year will have surgery for their epilepsy. “With improved diagnostic procedures and less invasive operative techniques, we have seen a steady growth in the number of surgical cases, from two to four pediatric surgeries per year six years ago, to 17 in 2023,” said Nordli. “But at the same time, we are discovering that many patients with intractable epilepsy have gene mutations that are causing their seizures, which surgery won’t fix.”
“But we're hopeful that our growing knowledge of the genetics of epilepsy will markedly improve pediatric epilepsy treatment in the near future,” Nordli added. “Currently we use broad-spectrum anti-seizure medications to control seizures, but soon we’ll be able to offer more tailored treatments, whether that’s small-molecule drugs or even genetic modifications.”
Other treatments under investigation include the use of lasers or focused ultrasound to ablate epilepsy foci and injections of human stem cells. “We will also be adding an fMRI-EEG machine, the only one in the region, which will enhance our ability to detect minute areas of abnormality,” said Nordli.
“I’ve been treating children with epilepsy for 35 years, and this is the most exciting era of my career because of all the research currently being conducted on epilepsy,” he said. “I’ve never been more hopeful for a cure.”
Children with epilepsy are comprehensively evaluated and cared for by a multidisciplinary team at UChicago Medicine. “Our patients may be treated by a team of physicians and surgeons, rehabilitation specialists, radiologists, EEG technologists, social workers, educational and child-life specialists, and nurses,” said Nordli. “It requires a coordinated effort from a dedicated team of people, along with the right tools and expertise, to provide the state-of-the-art care worthy of a level 4 epilepsy center.”
To better serve patients worldwide with rare causes of epilepsy, Nordli and colleague Samuel Volchenboum, MD, PhD, were recently awarded a grant from the Chan Zuckerberg Initiative DAF, an advised fund of the Silicon Valley Community Foundation, for a three-year project to establish an international epilepsy data repository. The initial goal is to collect information on specific gene mutations along with digital EEG studies in children with monogenic causes of epilepsy. The researchers will work closely with patient-established foundations to accelerate the pace of work.

Douglas R. Nordli, Jr., MD
Douglas R. Nordli, Jr., MD, is a child neurologist specializing in early-onset epilepsy and a co-director of UChicago Medicine’s Comprehensive Epilepsy Center.
Learn more about Dr. Nordli