Our Legacy of Cancer Research Excellence
For more than 50 years, the University of Chicago has been a leader in cancer research. Our scientists and clinicians have consistently expanded the boundaries of knowledge and transformed cancer care and prevention.
Seminal discoveries made at UChicago have stimulated the development and introduction of many of the cancer treatments used today. As the examples below demonstrate, many of the roots of chemotherapy, hormonal therapy, gene therapy and bone marrow transplantation can be traced to UChicago.
1930s - 1940s
Charles B. Huggins, MD, demonstrated that prostate cancers are dependent on hormones, work that earned him the Nobel Prize in 1966 and transformed prostate and breast cancer research and treatment.
1950s
1960s
1970s

1980s

1990s
2000 - 2004


2005 - 2009


2010 - 2014


2015 - 2019
Thomas Gajewski, MD, PhD, demonstrated the role of β-catenin signaling in tumor immune exclusion and PD1 checkpoint inhibitor therapy resistance, showing that the T cell-inflamed tumor microenvironment is a biomarker of response to immunotherapy.


2020 -

Cancer Luminaries
2024 is the University of Chicago Medicine Comprehensive Cancer Center’s 50th anniversary of National Cancer Institute designation, thus we are planning a year full of events to honor our past, communicate our present, and envision our future. Cancer Luminaries is our podcast to learn more about the lives and careers of our invited guests.
In this special episode, Camilla Frost-Brewer held a fireside conversation with two former directors and one current director to learn what it is like to lead a National Cancer Institute-designated Cancer Center and how they approached the opportunities and challenges of the role. Medical oncologist Richard L. Schilsky, MD, Director from 1991 to 1999, drove initiatives to modernize and organize the Cancer Center. Cancer geneticist and cancer biologist Michelle M. Le Beau, PhD, Director from 2004 to 2021, not only helped the Cancer Center achieve Comprehensive status, but she strengthened our programs in population research, created educational programs and enriched our community outreach. Physician-scientist Kunle Odunsi, MD, PhD, Director since 2021, is leveraging resources, advanced technologies and partnerships from across the University network to take a pipeline of discoveries to the clinic where they can make an immediate impact. Together, they reflected on what is unique about the intellectual environment at the University of Chicago and predicted where cancer research is going next.
[INTRO MUSIC]
[00:00:03.56] Camilla Frost-Brewer
Hello, and welcome to this recorded episode of Cancer Luminaries, our 50th anniversary podcast series for the University of Chicago Medicine Comprehensive Cancer Center. I am so delighted to be joined by three wonderful guests, our current Cancer Center Director, as well as two previous Cancer Center Directors. Thank you all so much for joining us. I would like to start off, if people are unfamiliar with who you are, to just introduce yourself to us. Tell us your name and the years that you were the Cancer Center Director.
[00:00:42.14] Richard Schilsky
I guess I'll start. I'm Rich Schilsky. I'm a medical oncologist. I was the Center Director from 1991 to 1999.
[00:00:51.29] Camilla Frost-Brewer
Excellent.
[00:00:53.45] Michelle Le Beau
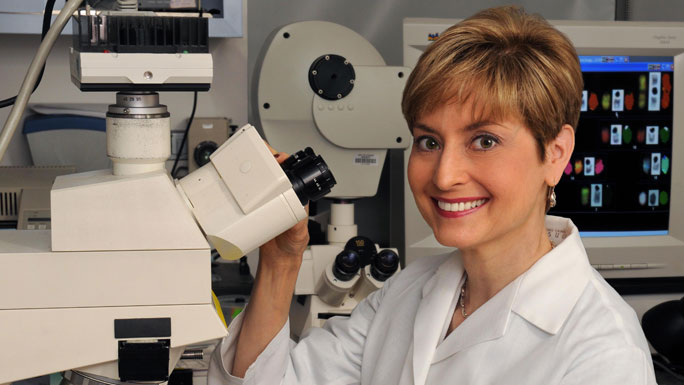
I'm Michelle Le Beau. I'm a cancer geneticist and cancer biologist and was Cancer Center Director from 2004 to 2021.
[00:01:02.79] Camilla Frost-Brewer
Excellent.
[00:01:04.23] Kunle Odunsi
I am Kunle Odunsi. I am a gynecologic oncologist. I also focus my research on tumor immunology and immunotherapy, and I've been Cancer Center Director since 2021.
[00:01:18.24] Camilla Frost-Brewer
Fantastic. And this is in 2024, just in case people listen to it later. So thank you all so much for being here. As I've shared, we do have some pre-arranged questions, so I'd like to just jump right in, really get to hear from you all what was it like and what is it like to be the Director for the Comprehensive Cancer Center. So our first question is, what inspired you to take on the leadership role of Director of the Cancer Center? What was your leadership style like during your time?
[00:01:47.82] Richard Schilsky
Well, I can start. I wouldn't say I was inspired to do it. I think you have to consider the times. It was 1991. The Cancer Center Core Grant [CCSG] was due for its competing renewal, and Dr. Ultmann, the founding Director, had neglected to submit the renewal application. And the grant was in a six-month, no-cost extension halfway through that.
[00:02:18.68] Camilla Frost-Brewer
Wow.
[00:02:19.42] Richard Schilsky
When the dean decided that perhaps a new Director needed to be put in place to bring some new energy and vision, I was identified-- I'm not exactly sure how-- as someone who might have the energy and the skills to do it. And frankly, I didn't really know what I was getting myself into, but I thought, OK, this is an opportunity to contribute to the institution. It's an opportunity to hopefully modernize the Cancer Center, make it more relevant to the cancer community at the University of Chicago.
[00:02:58.89] Richard Schilsky
And so perhaps somewhat against my better judgment, given the circumstances, I agreed, and then was informed that I had three months in which to prepare and submit a competing renewal of our Cancer Center Support Grant. So that was a challenging time. We can come back to that, if you'd like. It's part of ancient history now, but it forced a lot of things to happen.
[00:03:27.25] Richard Schilsky
It forced me to get to know the institutional cancer leadership better than I did, and it forced them to get to know me. It forced me to develop some vision for the Cancer Center, to develop an organizational plan for the Cancer Center that, frankly, wasn't in existence at the time, to take stock of what was necessary in terms of core facilities for the Cancer Center. All of this being necessary to have a chance at successfully recompeting the Core Grant, which we ultimately did.
[00:04:03.64] Richard Schilsky
Got it renewed. Unfortunately, at that time we the renewal was only for three years. So we had about a year and a half, and then we had to do it all over again.
[00:04:13.93] Camilla Frost-Brewer
The whole song and dance.
[00:04:14.90] Richard Schilsky
But the second renewal was much more successful and the rest is history.
[00:04:20.23] Camilla Frost-Brewer
Amazing. It's convenient that you all are sitting in chronological order, so thank you for that. Does anyone else want to comment about maybe what inspired you, drove you to take on this leadership role?
[00:04:35.03] Michelle Le Beau
I'll be happy to. When I took on the role as Cancer Center Director in 2004, it really was an opportunity. It was a challenge because we needed to rebuild many aspects of the Cancer Center, but it was a remarkable opportunity. And part of that was because of the preeminence of the university programs, the existing programs in the cancer programs, both for clinical care and research, but also an opportunity to take advantage of the remarkable programs throughout the university. And it was also a time when genomic medicine was beginning to emerge.
[00:05:13.56] Michelle Le Beau
So it was a remarkable opportunity for us to integrate that and to attempt to be leaders in that field. It was also challenging. I had a little bit more time than Dr. Schilsky to work with the faculty to prepare the Cancer Center Grant, but I think that as every new leader comes in, it is always a time for developing a new strategic plan, for reevaluating the programs, and developing new initiatives and goals going forward. So I had the great good fortune of being able to work with the faculty to do that. And we had about two years to get our Cancer Center Grant in, which proved to be successful.
[00:05:54.69] Camilla Frost-Brewer
Amazing. And Dr. Odunsi, if you'd like to comment as well as the current Director, having just submitted, successfully, a Cancer Center Support Grant. If you want to provide maybe some context to our listeners about what the CCSG is.
[00:06:10.17] Kunle Odunsi
So first of all, let me acknowledge my predecessors, two giants in the field. And also just to say that when I came, my first priority was, don't mess it up, because they've done a remarkable job building a Comprehensive Cancer Center. So let me start from what motivated me to take on this role. I was at a point in my career where I was looking for opportunity to make a bigger broad impact on cancer care, cancer research, and including community engagement. I was in a leadership role in my previous institution as deputy Director, and I was looking for such opportunities.
[00:07:02.02] Kunle Odunsi
And frankly, a number of institutions came my way that I could have gone to, but University of Chicago was so different. It has a strategic distinctiveness in its ecosystem, some of the things that Michelle talked about, with regards to how you have a world-class university sitting in Hyde Park with all of the attributes, everything, every ingredient that you need to make a major impact, breakthrough discoveries, breakthrough transformation.
[00:07:37.92] Kunle Odunsi
So it was easy for me to come to a decision to come to the University of Chicago to lead the Cancer Center. And with regards to the Core Grant, I immediately found out that I had to do the Core Grant, actually within one year. We appealed to the [National Cancer Institute] NCI. Even though one year is longer than three months, Rich, we appealed to the NCI to get an extension. So I had a period of two years to figure out how to put the grant together. It's a lot of effort, even within two years. I think you really need about three or four years to get it done properly.
[00:08:23.49] Camilla Frost-Brewer
Excellent. Thank you all for sharing. I appreciate the different ways you came to hold a similar position. I won't say it's the same because every Director is different. You all mentioned during your Directorship that there were many opportunities and challenges. So can you maybe talk to us about what was one of the greatest opportunities and one of the greatest challenges during your time.
[00:08:48.05] Michelle Le Beau
When I took over the position, there was an institutional vision to achieve comprehensive status for the Cancer Center, and I was very excited about that opportunity because it was an opportunity to recruit and build population research and community research efforts. I was able to build upon the initiatives that Dr. Schilsky put in place and the people that he recruited to begin to build population research. But we had to recruit a larger team, and that was within a period of two years, and to build a presence in population research and in community engagement.
[00:09:32.36] Michelle Le Beau
And that became an institutional goal. It became a priority for all of the leaders in the Cancer Center, and it became something that we all worked together on and everybody pulled together towards the same goal. So for me, that was both the greatest challenge, but probably the greatest accomplishment, because it changed the structure of the Cancer Center going forward. It created new opportunities at the NCI, the National Cancer Institute, which were not available previously to Cancer Centers that did not have comprehensive designation.
[00:10:07.19] Michelle Le Beau
It also created an opportunity for institutional support to allow us to engage in more community-based activities and to increase our effort in supporting the South Side community and other underserved populations in our catchment area. So I think that this was a remarkable opportunity and challenge, but something that I think everybody who participated in should be proud of.
[00:10:34.52] Camilla Frost-Brewer
While I was not there for that, that sounds like an amazing accomplishment and we thank you. I mean, we are still a Comprehensive Cancer Center to this day, so it's very exciting. Anyone else? Would you like to share your greatest opportunity, challenge?
[00:10:50.66] Richard Schilsky
Well, I will say this. When I assumed the Directorship, we really had to remake the Cancer Center to comply with NCI guidelines and expectations, which, frankly, had been largely ignored. Many people were listed on the membership roster but didn't know they were members of the Cancer Center. It was largely invisible inside the institution and externally. There was no signage anywhere to even indicate where the Cancer Center offices were.
[00:11:28.28] Richard Schilsky
I mean, it was a hidden program, both internally and externally. The basic science community, which was critical to the success of the Cancer Center, was not well-represented among its members. The reason it was critical is because the budget of the CCSG is linked to what's known as the research base. The research base is dependent upon the grant support that's garnered by the faculty, and the basic science faculty had most of the grants.
[00:12:01.46] Richard Schilsky
So one of my challenges-- and I was largely unknown to the basic science departments as a clinical oncologist. So one of the first things I did was I went around and I met in person with each chair of each basic science department. And I needed to understand from them who on their faculty was doing research that was related to cancer, and to make the case that the participation of their faculty in the Cancer Center would be value-added for them, for those individuals, for their departments, and to begin to get the basic science faculty engaged in the Cancer Center.
[00:12:47.81] Richard Schilsky
There were no formal programs in the Cancer Center at that time, even though those are required by NCI. There were four faculty who had large grants known as Program Project Grants. And because those grants were, by their nature, multidisciplinary and involved multiple faculty, they were sort of declared to be the Cancer Center programs. But they were still very limited in scope, and many faculty who participated in cancer research couldn't find a place in one of those programs. So we had to rejigger all the programs, the definition of the programs, and identify where faculty could fit.
[00:13:35.03] Richard Schilsky
I think one of the major responsibilities and opportunities for the Cancer Center Director is to make connections among faculty who would not necessarily gravitate toward each other. To do that, you have to understand what everybody's doing and you have to be able to envision how they might benefit from working together. And then you have to cajole, incentivize, twist arms, and so on to actually get them to collaborate. But if you can do that successfully, sometimes something magical happens because you bring together people from disciplines that wouldn't naturally have found each other. And that's sometimes where the spark really occurs.
[00:14:27.26] Camilla Frost-Brewer
Yeah, that sounds really amazing to be kind of the connector of all of those pieces.
[00:14:35.35] Richard Schilsky
Yeah. I mean, in one way, that's how I think of the role of the Center Director is to be the connector, to be the champion, to be the person who sets the vision for the cancer programs in the institution, and then hopefully aligns the resources to achieve that vision, and to be the champion for the institutional cancer activities in the larger cancer community. The Cancer Center Director, externally, is actually quite a visible role. The challenge is actually making it visible internally, which is not always so easy.
[00:15:20.77] Kunle Odunsi
I think the major opportunities-- well, I'm going to talk about two opportunities. The first one is what Rich already alluded to, and that is this opportunity to build teams, to bring people together. But then you need to articulate a compelling vision that people will align around, and then use these teams to accomplish greater impact.
[00:15:53.06] Kunle Odunsi
So one quick example is when I came in, I saw the strength of the Argonne National Lab, for example, which is perhaps one of the world's best institutions in terms of computational capabilities, in terms of ability for the Advanced Photon Source. And it jumped out to me right away, especially because this was around the time of COVID and they had done some work where they pull people together, the UChicago community, to discover new drugs, new COVID drugs.
[00:16:34.56] Kunle Odunsi
In fact, one of the investigators is on my floor in the lab, and described how Argonne and UChicago really came together trying to solve the problem of COVID. And I thought to myself, why can't we utilize this same strategy and focus on cancer? And made some contacts at Argonne, and I found very quickly that they were very excited to work on the cancer problem. So we initiated a platform or a process for drug discovery and development using their supercomputational capabilities. I mean, they can screen up to 1.3 trillion compounds, the limit of chemical space, within a matter of 30 minutes or so.
[00:17:27.11] Camilla Frost-Brewer
Wow.
[00:17:28.10] Kunle Odunsi
So we have a process now where we put a challenge to the Cancer Center membership to say, give us your best target. What are the targets that you are working on that potentially could lead to a breakthrough? Some of the targets traditionally are considered undruggable or difficult to drug, but we're finding compounds against these targets now. And that process is ongoing, likely to accelerate the discovery and development process for new drugs. So that was really something that I saw as an opportunity.
[00:18:08.27] Kunle Odunsi
And then the second one that I wanted to touch on is really this whole thing about cancer health equity. Again, coming in as a physician scientist, I think my first few weeks I was on service. I see Dr. [Diane] Yamada in the audience and Dr. [Nita] Lee. And I went on rounds, and I think I saw about three or four patients with stage IV, stage III cancer of the cervix. That should no longer occur in the United States. I did not see those types of patients in Buffalo, New York, where I was coming from. And 100% of those patients were from underrepresented minority populations.
[00:18:53.27] Kunle Odunsi
So that really hits me hard, that there is work to be done. So consequently, the opportunity is how-- so these are the problems, and working with Dr. Nita Lee, who is our Associate Director for Community Outreach and Engagement, were we to analyze the data showing that your zip code, the ZNA-- some people call it ZNA-- actually drives these disparities more than the DNA. And so what are we doing about this? A lot of outreach efforts now, again, led by Dr. Nita Lee and her colleagues.
[00:19:36.80] Kunle Odunsi
A lot of outreach efforts. We also established a center to address – the [Center to Eliminate Cancer Inequity]. So I'm very excited about the fact that we're really reaching out more than ever before to try and address some of these disparities. And I really think we could be the model for the nation in how to deal with this issue. It's not peculiar to Chicago alone. It's really all over the country.
[00:20:07.37] Camilla Frost-Brewer
Thank you. You heard it here, folks. UChicago, we now have the challenge to be the model. I want to touch back on the first example you gave, Dr. Odunsi, in my next question. What are or were some of the transformative discoveries in cancer research that happened during your time as Director?
[00:20:30.92] Kunle Odunsi
There are quite a lot of them. So let me start with one that stands out is actually the work of Dr. Jing Chen. I think it was published last year in Nature. Very elegant work where he focused on dietary metabolites and asked the question, how could dietary metabolites influence the behavior of immune cells, CD8-positive T cells? And he screened a battery of these metabolites and identified one, which, in fact, is not made in our bodies. You can find it in dairy products, beef, milk, and so on.
[00:21:17.05] Kunle Odunsi
I'm not suggesting you go out and start eating a lot of beef, but this was a very elegant study and showed that these metabolites called trans-vaccenic acid can promote responsiveness to immune checkpoint inhibitors. I'm very excited about this study, but with all things in terms of discovery to the clinic, we run into this wall, what I call “Valley of Death,” where we have a very nice, elegant study. We have a very strong publication. How do we take that to the clinic?
[00:21:56.90] Kunle Odunsi
And as Rich was pointing out, that's part of the job of the Cancer Center Director, to find an environment to create and foster and find resources to be able to take that to the clinic. So we're working on that. So, very exciting that you can have something in beef or in dairy products that you can then purify and potentially add to standard therapies, especially immune-based therapies. The second example is work by Lev Becker. So there's another group of cells called neutrophils.
[00:22:37.21] Kunle Odunsi
Typically in tumor immunology, we disregard neutrophils, that they don't do anything. We all focus on T cells, [natural killer] cells. Neutrophils are generally very useful in acute infections, but in fact, Lev made the novel observation that there is an enzyme released by these neutrophils that can actually help to fight cancer. It's called neutrophil elastase, and he actually code-named it ELANE. So this elastase has very strong activity against cancer cells, and he was able to show that by developing a drug that is similar to neutrophil elastase, you can actually cause tumors to regress.
[00:23:28.06] Kunle Odunsi
That project is going on to a clinical trial right now as we speak. So those are a couple of examples of important discoveries that are going on in the Cancer Center, and there are many of them going on. In fact, we have a rich pipeline of discoveries. I think our challenge is how to then make that transition and take them for clinical application. And that's something we're working on.
[00:23:58.12] Camilla Frost-Brewer
Right. That's only in three or four years. Wow. I'm very excited for the other answers. I do want to share-- this podcast is not about me, but I'm giving my parents a shout out because in our family chat we send a lot of news articles about various things, and they sent me an article about the study with beef and milk.
[00:24:22.22] Camilla Frost-Brewer
And I was like, oh, I actually know-- I mean, I don't know that person, but I know that name. I've looked at the membership roster endlessly, so that was pretty cool that they were like, wow, you work with these people. I'm not a cancer researcher, sadly. In another life. But it's really cool to be able to work with those people and see their work potentially change lives. Other discoveries?
[00:24:47.30] Michelle Le Beau
Sure. Well, those were tremendously powerful examples that you outlined, Kunle. I'm going to try to paint my examples with really broader strokes. During the years that I was Cancer Center Director, some of the fields that have emerged and had a big impact on our activities were artificial intelligence. An example is the work of Dr. Maryellen Giger, whose work led to the first program that was approved by the FDA for AI-guided screening mammography analysis programs, which have now-- since then, a number of programs and initiatives have been approved, but that's really revolutionized how mammography is done.
[00:25:39.89] Michelle Le Beau
I think another example is pharmacogenomics, which has also really changed how patients are treated, and I think is going to continue to help lead the area of very personalized medicine. People like Dr. [Eileen] Dolan and Dr. [Mark] Ratain had made major discoveries in that area. An additional area is the work done on inherited cancer susceptibility syndromes. People like Dr. [Olufunmilayo] Olopade in breast cancer had discovered a number of genes that are inherited in families and put them at risk of breast and ovarian cancer.
[00:26:21.62] Michelle Le Beau
Dr. Jane Churpek and Dr. Lucy Godley had done really seminal work and emphasized, really for the first time, that the hematologic malignancies also had a very large inherited component, something that we had not previously recognized. And they developed diagnostic panels that could be used to identify families with inherited predisposition syndromes. I think the last example that I'll mention also relates to the work that Dr. Odunsi mentioned, and that is tumor immunology and immunotherapy, which really just exploded during the time that I was Cancer Center Director. A number of individuals here contributed to that area.
[00:27:02.38] Michelle Le Beau
But I think some of the interesting work has been the work of Dr. [Thomas] Gajewski, whose work with animal models showed that the microbiome, the bacterial composition in our gut, can influence how we respond to immunotherapy. They went on to identify some of the types and strains of bacteria that can influence that process. That has led to a number of clinical trials to try to modulate that process. And really, the whole concept of trying to modulate the response to immunotherapy. So those are just a few examples of some of the remarkable discoveries made by University of Chicago faculty.
[00:27:44.64] Camilla Frost-Brewer
I laugh, just a few, like, changing the whole field. Again, exceptionally honored to be able to work with some of those folks still. I'm not sure if any of our questions touch on it, but I also really appreciate that some of those-- I can probably guarantee all of those researchers, but just in my short time here, have gone on to try to train the next generation as well. They don't just kind of let their research, their clinic work, end with them or the trainees they're assigned. They go out and teach the next.
[00:28:19.09] Michelle Le Beau
I think mentorship is really part of the culture of the University of Chicago Cancer Center and the university as a whole.
[00:28:27.05] Camilla Frost-Brewer
Yes.
[00:28:29.52] Richard Schilsky
It's actually very interesting to hear the examples given by Kunle and Michelle, because when I was the Director, it was, I think, a very transitional time in cancer science. The whole field of precision medicine hadn't yet really begun. Remember, I was the Director, '91 to '99. Herceptin was first approved by the FDA in 1998, so right toward the end of my Directorship. Imatinib was approved in 2001. And it's worth noting that both of those drugs were rooted in work done at the University of Chicago or by University of Chicago people.
[00:29:12.12] Richard Schilsky
One of my medical school classmates-- so I'm an alum of the Pritzker School of Medicine. One of my medical school classmates was [Dennis Slamon]. And Dennis, of course, is the one largely credited with identifying HER2 overexpression as a predictive marker for aggressiveness of breast cancer, which led, then, to the ultimate clinical development of herceptin as a highly effective therapy for patients whose tumors overexpress HER2. And of course, imatinib is directly rooted in Janet Rowley's work over many, many years here in discovering the BCL2-ABL translocation in CML [chronic myelogenous leukemia]. The BCL2-ABL translocation.
[00:29:59.80] Richard Schilsky
All of these discoveries that happened toward the tail end of my Directorship actually had some origin in the work of our own predecessors on the University of Chicago faculty. Not to mention hormone therapy for prostate and breast cancer, of course, which took root with the work of Charlie Huggins and discovering the work-- the role of androgen and the growth of prostate cancer and the work of Elwood Jensen in discovering the estrogen receptor, and so on.
[00:30:32.57] Richard Schilsky
And interestingly, Maryellen Giger, of course, was doing her work on computer-assisted mammography even while I was the Director. You may recall that we put together an advanced imaging program as one of our Cancer Center programs, which I think probably was the first imaging program in a Cancer Center in the country. And it was grounded in Maryellen's work, but then brought in a number of other faculty, largely from radiology, but also from physics and other places who were doing similar work, because AI wasn't on the scene yet.
[00:31:11.18] Richard Schilsky
But you know, her work led to, as Michelle pointed out, a device that could assist radiologists in interpreting mammograms, and subsequently in interpreting lung nodules and other things. Jeff Bluestone, who was here at the time working in immunology and ultimately became the Director of the Ben May Institute, was working on immune co-stimulatory molecules, which were important in the ultimate development of the immune checkpoint inhibitors that Kunle mentioned. And of course, I had the great fun of working with Eileen [Dolan] and Mark Ratain in developing all the pharmacogenetics work that we did here.
[00:31:57.85] Richard Schilsky
I came to the University of Chicago or returned to the University of Chicago in 1984, specifically charged with developing a phase I clinical trials program in the Hem/Onc division, which I did. And then when I became the Cancer Center Director, Mark Ratain took over the leadership of that program, and Mark's interest very quickly turned from just phase I clinical trials to understanding the genetic makeup of individuals that could influence their drug metabolism and drug clearance, and thereby their toxicity and effectiveness of their cancer treatment.
[00:32:34.42] Richard Schilsky
So I think we were at the forefront in those years in pharmacogenetics as it applied to cancer pharmacology. And it's now a much more well-established field, although still a lot to learn. So it was, I think, a transitional time in cancer science. But I can look back now and see how much of what came after my tenure was actually rooted in scientific discoveries that happened during my tenure or prior to it.
[00:33:09.60] Camilla Frost-Brewer
Right. Wow. I just need to take a moment. That's so cool. About 35 years of Cancer Center discoveries-- not all Cancer Center, but cancer discoveries at UChicago represented here. Sometimes people like things in chronological order. I love that we went backwards, because we heard what's happening now, and it's like, this has deep roots. And I really appreciate that. I want to go a little off script with you all, but I think you'll like the question.
[00:33:39.13] Richard Schilsky
At your own risk.
[00:33:40.23] Camilla Frost-Brewer
At my own risk. That's fair. I will take said risk. Dr. Le Beau, you mentioned that mentorship is really a culture at UChicago. I would like to hear from you all, who are some of your mentors that really stick out in your mind? Maybe that helped with your career trajectory, guided you on a path that led you to Cancer Center Directorship, influenced your research, et cetera.
[00:34:03.33] Richard Schilsky
So how did I become an oncologist? It was my decision to move in that direction. It was grounded both in personal family experience. My maternal grandmother, who I was very close with, had breast cancer-- actually, bilateral breast cancer, but at two different points in time. In those years, had two radical mastectomies followed by radiation therapy, and eventually developed metastatic disease.
[00:34:33.41] Richard Schilsky
There were virtually no effective therapies in those years except for tweaking the hormonal systems in various ways. And it was tragic to see her demise over a number of years while I was in college. So that sort of got me interested in the problem of cancer. When I was here in medical school, of course, Dr. [John] Ultmann was actually a very influential mentor to me, a very charismatic person, a leader in his field in lymphoma, and someone who sort of knew the ropes, knew what was necessary to develop a career in oncology.
[00:35:19.97] Richard Schilsky
And he actually advised me to think about eventually training at the National Cancer Institute. And so when I was a senior medical student, I applied for a fellowship two years hence at the National Cancer Institute and was accepted. Now, there was this little matter. At first I had to do an internal medicine residency.
[00:35:45.70] Camilla Frost-Brewer
A small matter.
[00:35:46.66] Richard Schilsky
Which I did at University of Texas Southwestern. And I then went on to the NCI and had there two very influential mentors, a man named Bob Young [Robert C. Young], who was chief of the medicine branch then, who was a seminal figure in developing new therapies for ovarian cancer and just was an outstanding clinical oncologist. And then I went in the laboratory of Bruce Chabner, who was the chief of the clinical pharmacology branch and, again, was an early leader in cancer pharmacology and biochemical pharmacology of antimetabolite drugs.
[00:36:24.52] Richard Schilsky
And it was through those experiences that I both learned some pharmacology, learned how to do clinical trials, and that put me on the path that I ultimately followed. So mentorship is incredibly important. It's important at every stage in your career. I still, in my later years in my career, return to some of these same people for advice at various times when I was trying to make important decisions. But I think it's those kinds of experiences that are extremely influential in one's life.
[00:37:08.95] Camilla Frost-Brewer
Thank you. Our communications Director really has her work cut out for her listing all these people. She's going to be so mad at me. But I love to share the work. You know?
[00:37:20.06] Michelle Le Beau
I had the great good fortune of having the ultimate mentor, Dr. Janet Rowley. How did that happen? I came here as a postdoctoral fellow in the early '80s. I did not intend to stay in cancer research. I wanted to learn about cancer genetics, but I expected to go on to do other types of genetic research. But within three months I knew I would never leave the field. And part of that was because of the remarkable opportunities that Dr. Rowley created for myself and so many other people that she mentored.
[00:37:55.33] Michelle Le Beau
She was really a remarkable mentor in terms of her generosity, creating opportunities for individuals, allowing them the freedom and independence to grow and to develop projects with just the right amount of guidance, just the right touch of guidance to keep you on the right track. She had a remarkable network across the world and used that network to benefit and advance her trainees. So really, a remarkable mentor.
[00:38:30.31] Michelle Le Beau
I think what was most important was the love of science that she instilled in all of her trainees. But as Rich said, all of us have many mentors along the way, and I was also very much very fortunate to benefit from being mentored by Dr. Harvey Golomb, Dr. John Ultmann, and Dr. James Vardiman, and remarkable collaborators.
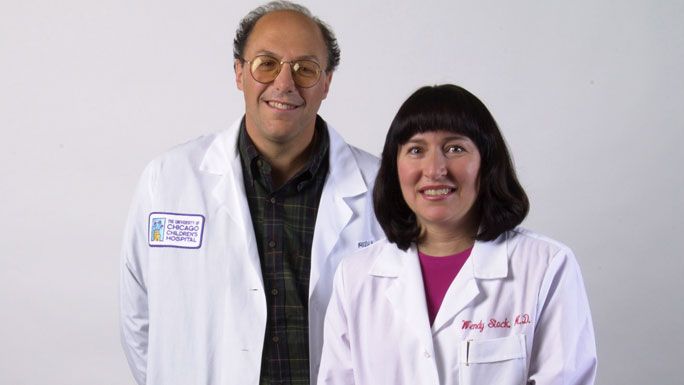
[00:38:57.90] Michelle Le Beau
I was able to work with Dr. Richard Larson for 40 years, as well as people like Dr. Wendy Stock, who have directed our leukemia programs. And really, I learned very quickly that one of the most unique things about the University of Chicago was the caliber of your colleagues who make you better than you would otherwise be and create opportunities for you. And I think that all of us have benefited that type of opportunity.
[00:39:36.42] Richard Schilsky
The other thing that's important is the quality of your mentees and your trainees who challenge you every day to live up to their expectations, to help them become successful in their careers, and who, if you got the right trainees who were extending into areas of science that you may be less familiar with, but where your experience can still guide them to success in their own research.
[00:40:11.61] Camilla Frost-Brewer
Right. Thank you.
[00:40:14.67] Michelle Le Beau
Good point.
[00:40:15.16] Camilla Frost-Brewer
It's a symbiotic relationship.
[00:40:16.96] Richard Schilsky
Absolutely.
[00:40:18.03] Camilla Frost-Brewer
Thank you.
[00:40:19.65] Kunle Odunsi
I could go all day listing my mentors, mentors at every stage. I'm going to pick one mentor, particularly, that stands out. There are many. Maybe I'll speak about another couple. But the mentor that really stands out-- this was after I had-- I was starting as a junior faculty, and it was very clear to me that I wanted to take a physician scientist path, to have a lab but also do my clinical work.
[00:41:00.13] Kunle Odunsi
In gynecologic oncology, you have to do surgery. We administer chemotherapy. We're doing our clinical trials. So you can imagine how busy that could be. And yet, I wanted to have an independent research lab. So I was trying to figure out, where do I start from? It was very clear. So as I was getting ready for this, I was able to nail down what I wanted to do.
[00:41:30.76] Kunle Odunsi
But the person that really originally drove the concept was someone by the name Lloyd Old. Lloyd was the Director of the Ludwig Institute for Cancer Research, as well as scientific Director for the Cancer Research Institute in New York. The Ludwig Institute is a huge network around the world. I mean, branches in Australia, in Europe, in the UK, Switzerland, Brazil. He was directing this big enterprise.
[00:42:08.41] Camilla Frost-Brewer
Wow.
[00:42:08.68] Kunle Odunsi
And so I gave him a call. Remember, as a junior assistant professor, called Lloyd Old. Lloyd had been nominated for the Nobel Prize. So called Lloyd Old and asking him, can you share this antibody that you discovered in your lab a couple of years ago? I want to test it on ovarian cancer. That was my question. He wasn't around. Then I called back. He wasn't around. And then finally, I called the first author on his paper, Achim Jungbluth, and he picked up the phone.
[00:42:52.94] Kunle Odunsi
And I said, I need this antibody. I want it to test. And he said, let me check with Dr. Old. If it's OK, then we'll send it to you. Cut long story short, I got the antibody, tested it in ovarian cancer. Then I called back to say I have some results. I want to share the results and see how we can publish a manuscript. And when I called Achim, he said, Dr. Old is here with me right by my side, and then handed Dr. Old the telephone.
[00:43:26.78] Kunle Odunsi
And he said, I think you need to come to New York to come and present your results. So I went to New York, presented the results. This was simply immunohistochemistry at the time, but it was a big deal. That was the only group that had the antibody that I was looking for. After the presentation, he actually pulled me to his office. So the presentation was in a boardroom at the Ludwig Institute. And pulled me to his office to say, look, I think I know what you're looking for.
[00:43:59.16] Kunle Odunsi
I'm going to mentor you. I know that you want to help your patients potentially with a vaccine. I'm going to mentor you to see how you go forward. That was the beginning of a very important relationship, not just mentorship, sponsorship, and really caring not just about the science, but caring about you as a person. He knew my family. We would talk for-- this is Dr. Lloyd Old.
[00:44:38.81] Kunle Odunsi
And so sponsorship is important as well because-- so he was able to position me for opportunities. So, for example, I need protected time for my research. He was scientific Director of CRI, Cancer Research Institute. There was a fellowship that could protect 75% time for a clinical investigator. He was able to help me to make sure I was able to receive that fellowship, and that left me with 75% protected time of lab time in those very early years.
[00:45:17.75] Kunle Odunsi
So mentorship, sponsorship. So that's the one big example for me until he passed away in 2012. Let me quickly give a second one, and that is-- so I transitioned from the United Kingdom. I had my first residency training, my PhD training in England. When I was transitioning, just like Rich, I was looking to do a fellowship in gynecologic oncology in the United States. But there's only one wrinkle. I had to come from an ACGME-accredited residency program.
[00:45:56.48] Kunle Odunsi
I had completed my first residency, so I had to repeat my residency in the United States. But Dr. Fred Naftolin, the chair of OB/GYN at Yale, where I did my residency, accepted me to the program, a four-year program, and also mentorship. So he said, I know you are an unusual resident because you already completed one residency training program. So we're going to create time for you, and I know what you're looking for.
[00:46:32.52] Kunle Odunsi
So he actually mentored me to create time for me to be able to continue to do some research during a very busy surgical-- OB/GYN, it's a surgical program. A very busy residency training program, which I appreciated. So I remain in touch with Dr. Naftolin up till the present day. So those are just examples. Let me end by just saying that having experienced mentorship at every stage I take-- and I think we've already heard about this, and all of the folks at UChicago, we take mentorship very seriously.
[00:47:14.23] Kunle Odunsi
In fact, the Cancer Center, we have a mentorship committee that is led by Dr. [Susan Cohn] here. She actually assigns mentors to junior Cancer Center members, making sure they are on track and making sure we create opportunities for them. I believe that to whom much is given, much is expected, and I hope I live that each and every day.
[00:47:44.67] Camilla Frost-Brewer
Amazing. I knew you all would want to talk about your mentors. Had to throw the question in. I'm going to switch gears a little bit back to the Directorship. And I think we can all agree that we know a Director of such a large matrix center is the connector, as we've mentioned. But what is one thing that people don't know about being the Cancer Center Director? I'm limiting you to one.
[00:48:14.68] Richard Schilsky
Well, it depends on whether you're asking about people internally or externally.
[00:48:21.22] Camilla Frost-Brewer
Good question.
[00:48:22.06] Richard Schilsky
And of course, my answer will be based on my experience 34 years ago and so on. But I would say that one of the things that is now or at least was then misunderstood is that in a matrix center, the Cancer Center Director has a lot of responsibility but often very little authority.
[00:48:46.39] Richard Schilsky
And that makes the job particularly challenging because there are high expectations, usually by leadership, for what the Center Director and the Center itself can accomplish, usually grounded in “Make sure the Core Grant gets renewed!” That's the highest level of accomplishment that most institutional leaders are really interested in. But because of the way in which NCI has set expectations now for institutional commitment and the responsibilities of the Director, having more authority is, I think, vitally important.
[00:49:34.22] Richard Schilsky
I came into the Directorship role at a time when I had no appointment power. I couldn't hire any faculty. They all had to be hired in departments. I had no laboratory space that I had under any control. I had a small amount of money that I had to get a commitment from the dean that if I raised money for the Cancer Center, that it would stay in the Cancer Center, which was also a challenge.
[00:50:01.13] Camilla Frost-Brewer
OK, working with a full band here.
[00:50:03.26] Richard Schilsky
I didn't have a whole lot to work with to incentivize people to devote time and effort to the Cancer Center. And I think that's partly where the skillset, in a sense, of establishing a vision that perhaps people hadn't seen, creating opportunity. We talked about the Center Director being a connector, and I think from Michelle and Kunle's comments, I mean, I think the other word that really comes to my mind is catalyst.
[00:50:35.28] Richard Schilsky
It's the Cancer Center Director whose job is to be the catalyst for initiating new cancer research collaborations in the institution, and maybe that's the currency that we have to deal in, even if we don't have some of the other responsibilities or other authorities and resources that might be available to Center Directors of a freestanding Cancer Center where presumably the Cancer Center Director there-- and I used to be on the external advisory board for Roswell Park, which is where I first met Kunle. That's a freestanding Cancer Center. The Director there presumably has a lot more authority, as well as all the responsibilities, that all the rest of us have had.
[00:51:25.49] Camilla Frost-Brewer
That's a great point. Thank you.
[00:51:27.15] Michelle Le Beau
I'll just expand on what Rich has said. I think that many people don't realize that the Cancer Center's program is a very unique program within the NCI and within the NIH [National Institutes of Health]. There are very few examples of a medical discipline or scientific discipline that has designated centers throughout the nation and are provided resources to develop those programs within the institution.
[00:51:57.84] Michelle Le Beau
And that is what the Cancer Center grant is really designed to do. And so the Cancer Center really serves as the umbrella organization. Cancer research is a broad field and cancer care is a broad discipline, occurring in many different departments across the university. And the Center acts as the umbrella organization to coordinate those activities and to catalyze new initiatives that bring people together to create new programs.
[00:52:27.71] Michelle Le Beau
But I will also say that what other people don't realize is that we have a secret club. We have our own handshake. No, but it is a very close-knit group of 70 some Cancer Centers now who really work together to help catalyze activities across the nation. And I think that's an important aspect that people may not recognize.
[00:52:54.29] Camilla Frost-Brewer
Thank you.
[00:52:56.55] Kunle Odunsi
I think what people may not recognize is the fact that sometimes it appears as if the world is falling on the Cancer Center Director, that everything is, because, whether on the clinical side or the research side, I get emails about problems, a lot of emails. And sometimes, it's like everything is falling apart. But what people may not know is that many Cancer Center Directors are still very passionate and excited about what they're doing.
[00:53:43.92] Kunle Odunsi
So we can encounter hundred problems a day, but what I have found is that it doesn't-- I mean, it doesn't faze many of the Directors when I listen to their experiences, and my own personal experience as well, that problems can be solved. And going in with that kind of attitude, I think, helps with the job. But in general, I think the challenges that we face are mostly where people are asking questions about resources, and sometimes it's beyond the scope of the Cancer Center.
[00:54:36.85] Camilla Frost-Brewer
OK. To summarize a little bit, we have that Cancer Center Directors are not only connectors, but catalysts who maybe the currency they deal in are opportunities and a strong vision and mission. We also have that there's a strong network of Cancer Centers across the nation. We are mighty in number now. And then that Cancer Center Directors have limited time but great passion.
[00:55:06.16] Camilla Frost-Brewer
I think that's phenomenal. Let's write it up, everybody. That's our marketing pitch. There it is. So we talked about mentorship a little bit, and I imagine some junior faculty will listen to this podcast, either watch it or listen on Spotify or Apple Music. We might have to cut that, actually, because I don't know if I can say that anyway. What is some advice you would give to junior faculty if they are aspiring to leadership in a Cancer Center?
[00:55:38.55] Kunle Odunsi
Well, I think what you've heard is that there is no prescription on how to get there, but there are some principles that I think could help. So the first principle is really to be involved in activities at a very early stage. Leadership activities. When I say leadership, it doesn't really mean to be appointed to a position. It doesn't mean a title. It simply means demonstrating leadership capabilities, bringing people together.
[00:56:18.26] Kunle Odunsi
And some people ask, what is the right timing? And I know a lot of people struggle with, should I wait till I get my tenure, my promotion. I think it should be incorporated very early on into-- and someone who aspires to do this, it should be incorporated at a very early stage. My own example, even as junior faculty, I was organizing departmental tumor boards, for example. OK?
[00:56:52.85] Kunle Odunsi
You may think that's something small, but in fact, it begins to help me to understand how to arrange, how to be organized. I was organizing departmental seminars, seminar series, the topics for those seminars. Actually, the first time of getting into Cancer Center programs, suddenly-- I think, Rich, you must have been at that meeting at Roswell Park.
[00:57:26.31] Kunle Odunsi
So I was called to the office of the president and CEO of Roswell Park at the time to say, we want to appoint you as the co-program leader for tumor immunology and immunotherapy. This was just, like, out of the blue. And I had no idea what that meant. And then the EAB [external advisory board] was coming, including Rich. I think the EAB was, like, a few weeks, like four weeks, and I was asked to provide a couple of slides. And then I stood up at the EAB meeting and they asked me, what is your vision?
[00:58:11.70] Kunle Odunsi
And I'm sure I said something, and suddenly they clapped and they said, that sounds good. So there is really no prescribed path. I think everyone's path is going to be different, but the principles are to be engaged, to be ready to volunteer. I know there are 24 hours in the day, but there are some things that kind of set you up for this kind of leadership opportunity eventually.
[00:58:43.14] Camilla Frost-Brewer
Excellent.
[00:58:43.71] Michelle Le Beau
I couldn't agree with you more. I think you have to take opportunities throughout your career. Nobody goes from being no leadership activities at all to being a dean. Each of us have had multiple leadership roles along the way, and you benefit and learn from each one of them. I would also say in my day they didn't have executive leadership training programs, and I would have loved to have taken advantage of those programs.
[00:59:15.30] Michelle Le Beau
So I would encourage people who think they may be interested in leadership to take advantage of those programs. But also to take advantage of the new communications opportunities that they have to teach you how to communicate your message, how to talk about science to a lay person, and get across the excitement in just a 30-second elevator speech. And I think these are really important opportunities to take advantage as you're coming up through the ranks. They'll benefit you in many ways that you may not appreciate initially.
[00:59:52.26] Richard Schilsky
I don't think I have much to add. I don't think there's necessarily any secret sauce. I mean, I get this question from young people all the time. And I basically say, first of all, show up. Second of all, speak up. Third of all, stand up, volunteer, and make your skills known, make your views known, make your ideas known. Fight for what you believe in.
[01:00:20.18] Richard Schilsky
And if you're able to do that, others will see in you the opportunities or the beginnings of a leader, because in my view-- and I've had quite a few leadership roles over the years, but they all reduced to a certain skillset, which in my view is, first of all, you have to be humble. Being the leader is about the success of the organization you're leading, not about your personal success. You need to put your organization ahead of your personal ambitions.
[01:01:03.99] Richard Schilsky
Second of all, you have to, as we said up here already, you have to have a vision for where you want or you think your organization can go and where it can have the greatest impact. After that, the rest is really about assembling the resources and identifying the people who can help you achieve your vision and letting them do the work and guiding them along the way to keep them on the path that you envision for the organization.
[01:01:38.91] Richard Schilsky
And I've found that sort of following those guiding principles, you can be successful as a leader in any organization. Each one will have its unique challenges. But at the end of the day, that's what the leader is about. That's, to me, what it means to lead. Look to the future. Figure out how you're going to get your institution from where it is to that desired future state, and then find the resources and the people to move it there.
[01:02:11.13] Camilla Frost-Brewer
I think that's so indicative of the leaders that you all are, that you-- a core component of what you all said was that leadership isn't just about the individual. It's about all of the people around you that help you get there, that you're leading, the vision and the mission that you all bring to the people. They have to get on board, right? Because if they're not on board, you're leading an empty building. So I think that shows the strength in the leadership.
[01:02:42.72] Camilla Frost-Brewer
I have one final question for you. Official question, of course. You never know. You might say something really astonishing and I'll go off on a tangent. But I think this is a really important question to end on, especially as we're doing this podcast for the 50th anniversary of NCI designation. What makes the University of Chicago Medicine Comprehensive Cancer Center special or unique? What sets us apart, maybe even above the rest?
[01:03:13.81] Richard Schilsky
Maybe I'll just start briefly, because, again, I think my experience may be a bit different from Michelle and Kunle's more recent experiences. But I think one of the things that has enabled the University of Chicago Cancer Center to be successful over the years is an inherent feature of the University of Chicago, which is multidisciplinary collaboration. Interdisciplinary work is a feature of so much of what goes on here. I mean, when you just think about the structure of the University of Chicago, very few places have the structure that we have, with the various divisions of the university.
[01:03:59.56] Richard Schilsky
And within the BSD [Biological Sciences Division], at least there are very few, if any, other institutions that I know of that have created the committee structure that we have where the committees, by design, are interdisciplinary, multidisciplinary, with the goal of bringing people together to work in a thematic area. And that's an inherent feature of the Cancer Center, of course, and that is something that has been a part of the U of C for many, many, many years. And I think that has been an enabling feature that the university has supported that has allowed the Cancer Center to be successful over the years.
[01:04:48.60] Michelle Le Beau
I share Rich's view, and I think it comes back to the core values of the university and the Cancer Center. It's the caliber of the people. It's the spirit of collaboration and the interest in multidisciplinary science. But I think there's a core value that I took for granted, as I spent my entire career here at the university. I realized that I took for granted the fact that university faculty and students are open-minded.
[01:05:24.78] Michelle Le Beau
They are always interested in hearing new ideas and thinking deeply about those ideas, thinking about how those ideas apply to their own situation, how you refine those ideas, and incorporate them into your own situation to come up with a better product, a better outcome. I did not fully appreciate that until I went out into the real world, I left the university, and I discovered that it's not that way everywhere. That you really begin to appreciate the open-minded and interest in having a dialogue and discussion and thinking deeply about new ideas and opportunities.
[01:06:08.24] Kunle Odunsi
Yeah, I think this is a special place for a number of reasons. Number one is the-- I think we already talked about the ecosystem here. This Cancer Center is able to take advantage of one of the best schools of molecular engineering [the Pritzker School of Molecular Engineering], the Booth Business School [Booth School of Business], which we are leveraging to address the issues of cancer health disparities, the Social Sciences and Policy School [Division of the Social Sciences, Harris School of Public Policy], which we're leveraging for disparities, the Physical Sciences Division. I mean, it is just a rich environment.
[01:06:46.53] Kunle Odunsi
The intellectual capacity, I think, is second-to-none, and all concentrated on this campus. So that's number one. Then number two is the people, which Michelle already talked about. We have incredible people always open to new ideas, collaboration. I mean, even with my schedule that is so busy, I get requests and I have a very small lab now. I scaled down my lab. I have requests to collaborate from so many people. That is so unbelievable. So that is the second component.
[01:07:33.85] Kunle Odunsi
Then the third is the leadership. I've been fortunate to be able to assemble a very strong leadership team. Our associate Director, our deputy Director, Dr. [Eileen] Dolan, the associate Directors, the program leaders, and others who are playing key roles in driving the direction of the Cancer Center. So we have the people, we have leaders, we have people who are selfless, who are passionate about trying to cure cancer aligned with the vision, overall vision to eradicate cancer and reduce health disparities. So.
[01:08:15.93] Camilla Frost-Brewer
Right. I may have fibbed a little bit. I do have one more question for you, and Dr. Odunsi, I think it speaks directly to the last part of your comment. Where do you all envision cancer research and care going in the next 50 years? So it's a lot of time. I know.
[01:08:38.97] Richard Schilsky
I think it's hard to envision where it's going to be in 10 years from now, let alone in the next 50 years. I mean, because the pace of discovery, has so much accelerated in the last 30 years in particular. I mean, we've learned more about cancer even in the last 20 years than we probably knew in the hundreds of years before that. And I think the pace of discovery is only going to continue to increase with as we introduce new technologies and so on.
[01:09:14.28] Richard Schilsky
We have a big challenge that I think Kunle is very focused on, which is making sure that everyone who could benefit from our available cancer treatments has an opportunity to receive those. It's been estimated that we could reduce cancer mortality by 20% to 30% if everybody who could benefit from a treatment actually could receive that treatment. We don't have to discover anything new. We just have to be sure that everybody can get access to the treatments that we have today.
[01:09:49.40] Richard Schilsky
That said, of course, not everybody is going to benefit from those treatments. We still have to have new discovery. It's always rooted in basic science, which is the critical underpinning of everything that we do. But what I think is necessary to happen is that cancer treatment will have to become increasingly more personalized as time goes on. Each person's cancer is unique. That much is clear. And even though we now have the tools to say, OK, you should have this treatment to match to your genomic target and your kind of cancer, that's only the tip of the iceberg.
[01:10:37.99] Richard Schilsky
Because even with that ability to match patients to treatments, we still have many patients who don't benefit because the biology is far more complex than that. So we're going to need to continue to sort that out. I hope it's going to lead to more and better therapies. We're going to need AI, we're going to need computer-assisted algorithms. The knowledge that's necessary to get cancer care to the next level is probably beyond the capacity of the human brain without some level of assistance. And I think that's where we have to be aiming, in my view.
[01:11:18.99] Michelle Le Beau
I appreciate the points that Rich has raised, and I'm only going to expand on two points. I think the issue of being able to expand the implementation of what we know into the community and to benefit all individuals is extremely important. It's very hard to do. So it's one of the reasons I'm so excited about the new center that you've started, and I hope I get the name right, The Center for the Elimination of Cancer--
[01:11:46.35] Kunle Odunsi
Health Inequities.
[01:11:46.62] Michelle Le Beau
Health Inequities. Thank you. I think that's really timely and just is essential. I think the second area that we will see enormous advances in the future is in the area of early detection and screening.
[01:12:06.34] Michelle Le Beau
And I think that tests like the multi-cancer early detection tests, which are under development now-- there's still a ways to go to develop these tests and to implement these tests, but the goal is to develop simple tests based on a blood sample or a urine sample that can detect multiple forms of cancer and could be made available to all populations for a lower cost than some of the current screening tests that we have now, an additional advantage being that they would screen for some of the cancers that we do not currently have traditional screening approaches for. So these tests, as I said, have a ways to go before they're ready to be offered to the general population. But they're very promising for the future and could be game changers.
[01:12:55.50] Kunle Odunsi
Yeah. So I completely agree with all of those points by Rich and Michelle. I'm just going to add one layer, which is going a step further to say prevention.
[01:13:10.84] Kunle Odunsi
I think in the next 50 years, as soon as you are a baby, we probably have your whole genome sequenced and be able to predict your risk of cancer. And what age. And the reason I say that is there's so much going on now in terms of Big Data. We're accumulating a lot of data, and with AI technologies, we should be able to predict who is going to develop cancer right at the time of birth, 50 years from now. And then because I see the world through the lens of the immune system, we should be able to design vaccines to prevent all forms of cancer. So that's where we're going to be in 50 years.
[01:14:00.82] Camilla Frost-Brewer
Excellent. Big, big vision there. I love it. I want to thank you all for answering my questions so far. But now we are going to go to three audience members who have prepared questions for you. So we will begin with Dr. Soni Smith.
[01:14:20.67] Soni Smith
What do you see as the biggest challenges furthering science going forward in the future? And are there lessons to be learned from the past?
[01:14:29.40] Richard Schilsky
Well, there's always that little thing about funding. I mean, the scientific community can gorge itself on every last dollar that's available and still need more. So I think as advocates for science, we all have an important role to play to be sure that funding levels are expanded to the greatest extent possible, because it's the funding that enables the research that delivers the breakthroughs. I think we need more in the way of public-private partnerships.
[01:15:18.29] Richard Schilsky
There's a huge amount of R&D investment by private industry, far more than what NCI and NIH invests, and it's largely proprietary. And it's not always easy to translate that into work that the academic community can capitalize on or the clinical community can deliver to patients if there's not a regulatory approval at the end of the path. So I think those are, in my mind, two important issues that we have to continue to work on.
[01:15:54.99] Michelle Le Beau
I would add to that by saying workforce issues in the context of training clinical researchers, physician scientists, basic researchers, translational researchers. I think our incentives are not fully aligned in terms of facilitating the work that these individuals do and ensuring that they have the training opportunities, but also can come out of these experiences looking forward to a reasonable future in research without accumulating just inordinate amounts of personal debt through this process.
[01:16:38.47] Kunle Odunsi
Yeah. I also think funding is number one, because even as of today, the NCI budget is diminishing. The potential to get your first R01 [grant mechanism] is diminishing. So funding is going to be number one issue. And then the second issue is the ability to translate discoveries to the clinic has become more and more expensive. I think we gave some examples of new discoveries coming out of UChicago, but we struggle with the transition from discovery to translation. So translation to clinical trials, for example.
[01:17:27.29] Kunle Odunsi
So for you to get IND [investigational new drug application] for a first-in-human study is so expensive. And so I think we’ll need to address that as a society. I mean, the FDA, rightly so, they do their job. They are protecting the public. They pay attention to safety. But some of those things that they require are so onerous that it's going to be difficult for us at the pace of discovery that's going on right now to try and test these things in the clinic. So I think that's going to be a challenge over the next several years that we will need to overcome.
[01:18:09.86] Camilla Frost-Brewer
Thank you. And thank you, Dr. Smith. Our next question is coming from Dr. Marcia Tan.
[01:18:17.27] Marcia Tan
Directorship of a Cancer Center is a complex leadership role. What type of skills do you need to cultivate to be an effective leader and how did you go about cultivating those skills?
[01:18:30.25] Kunle Odunsi
I think there are-- it's multifaceted skills, but I will start by saying basically a lot of common sense. Some things are just common sense. But clearly you need to cultivate some of those leadership skills that we talked about. And when I think of some of my mentors in terms of leadership, what do I look for in a leader? What do I look for in them? Things like trust, integrity. They project confidence, ability to articulate a vision, fairness, listening, ability to listen, respect everyone, and make sure that everyone's ideas are taken into account.
[01:19:24.55] Kunle Odunsi
And I think Rich mentioned humility, kindness. So those are all features which, again, there is no prescription for how to acquire them. Those are things that you acquire as you go along, along the line, along the path. Do you make mistakes along the way? Absolutely. Are there things I look back and I say, maybe I shouldn't have said that. Maybe that's not respectful enough. Absolutely. But as time goes on, you mature and you learn from those mistakes and hopefully take corrective actions.
[01:20:05.87] Michelle Le Beau
I think I would wrap up all of those traits that you just mentioned, Kunle, under emotional IQ. I think that most people don't realize that as a Cancer Center Director, you have many different stakeholders. You have the dean, you have the faculty, you have donors and the fundraising component that you're working with, and you need to find a way to communicate and develop a relationship and an understanding with all of those individuals. All of them have different goals and different needs, and you're trying to meet all of them.
[01:20:48.32] Michelle Le Beau
And you have to develop the skillset and the desire to put your own needs aside and to recognize that you are working for the greater good. You're working to advance the research programs, the clinical care programs, and to benefit patients and their families. And I think that once you-- if you think about your career, your first, it's really working to grow your own professional growth, and all of a sudden you make that transition where you are working now for the greater good. And I think it takes a certain amount of emotional intelligence to be able to make that transition and to do it successfully. But it takes all of those skills and traits that Kunle mentioned.
[01:21:38.92] Richard Schilsky
I don't think I have much to add. I mean, I think the communication skills are absolutely essential in a role like a Center Director, because you have, as Michelle said, so many different groups that you're speaking with. You have to have a broad appreciation of science. Most Center Directors, of course, have a particular area of their own scientific expertise, but that's not their job.
[01:22:04.25] Richard Schilsky
The job of a Center Director is to understand and value all of the domains of science that are represented in their Cancer Center and to be able to describe them to all of the stakeholders, because you never know what part of the scientific agenda of your Center is going to get traction with the audience you're speaking to. And so I think that's important, and I think as we probably have all experienced, being a Center Director is more about managing up than managing down.
[01:22:44.72] Richard Schilsky
The people that are members of the Center are generally pretty self-sufficient, pretty smart, pretty much on a successful career path. And what the Center Director really has to do is to continue to demonstrate to the organizational leadership the value of the Cancer Center and what it is bringing to the institution, more so than just the money in the Core Grant. The money in the Core Grant is nice to have.
[01:23:17.39] Richard Schilsky
But for most Cancer Centers, certainly for the freestanding Cancer Centers, the amount of money in the Core Grant is a tiny sliver of their Cancer Center budget. You might say, well, why do they even bother, because that amount of money is trivial compared to their overall Center budget? And they bother because it's a reputational issue, and that imprimatur from the NCI of being an NCI-designated Center is so influential in so many different spheres.
[01:23:56.15] Richard Schilsky
But it's up to the Director to communicate that. You may have an organizational leader, whether it's your dean, your president, or so on, who has no idea about cancer, is likely outside of the medical school environment, is likely not going to be a physician. And to be able to explain to them why the Cancer Center is unique, why it's important, and why they should commit resources to it-- that's the most important thing-- is a big part of the job. And so I think honing those communication skills and delivering that message is really important.
[01:24:38.46] Camilla Frost-Brewer
Thank you. And our final audience question will come from Dr. Eileen Dolan.
[01:24:45.48] Eileen Dolan
As we have this unique opportunity to have two previous Directors and a current Director of the Cancer Center, I'd like to know what your legacy was or would like to be.
[01:24:58.70] Richard Schilsky
Well, I've been thinking about this. And to be blunt, I think my legacy is probably saving the Cancer Center from its near demise and putting it on a path to success. And certainly those who've come after me have really accelerated the growth of the Cancer Center. I'm proud of the fact that the programmatic structure we put in place back in the early 1990s is still largely the programmatic structure of the Cancer Center today, which suggests to me that we did it the right way back 35 years ago and that the structure is still relevant to today's faculty and today's science.
[01:25:53.22] Richard Schilsky
But frankly, I think, given the challenges we had back in the early '90s, there was a real risk that the CCSG would be lost. And I can tell you from many years of serving on the parent committee of Cancer Center external advisory boards, and so on, it's actually pretty hard to lose a Core Grant. It's very difficult to get a Core Grant. It's also somewhat difficult to lose a Core Grant if the institution is paying attention to what's going on and making a commitment.
[01:26:28.50] Richard Schilsky
But it has happened. There are certainly examples where Centers have lost a Core Grant, and it's oftentimes very difficult to get it again. It can take decades of rebuilding. So the fact that our Center was in a somewhat precarious position when I assumed the Directorship and we were able to get it back on track and position it for success going forward is something I'm pretty proud of.
[01:26:57.06] Michelle Le Beau
Well, I was fortunate to have benefited from Dr. Schilsky's efforts to stabilize the Cancer Center and-- no, and to create new opportunities that we were able to leverage. So I would say that my legacy will probably be working with all of the faculty to secure Comprehensive status for the Center, to elevate us to the next level, and to create new opportunities for the Center through that designation.
[01:27:24.96] Kunle Odunsi
I am fortunate to build on the legacies of my predecessors. But I think where we are today with our science, I think there are two major areas that I think I would love my tenure to be remembered for. One is in therapeutics. We have unique capabilities for drug discovery and development, and I think I talked about that earlier. I really believe we have an opportunity to make some real breakthrough impact based on the infrastructure and the people at the University of Chicago.
[01:28:11.08] Kunle Odunsi
The second area that I think I would love to be remembered for is in the area of addressing cancer health disparities in South Side Chicago. We're putting programs together. Again, we have the right people in place. Dr. Nita Lee is leading that effort, along with Jasmin Tiro, who is not here this morning, to really make a difference, to make an impact. Health disparities. There are tons of papers. People have made their career writing papers about this. We know it exists. What are we doing about it? And that's where we're going to be different. And I think that could be a legacy for this tenure.
[01:28:54.97] Camilla Frost-Brewer
What a great question to end on. I feel so honored to be able to sit here with all three of you. So thank you for taking time to sit with me, to sit with the folks in the audience, and to be recorded for others to listen as they are able to for many years to come, we hope. We want to thank you deeply from the Cancer Center for joining us for this podcast, agreeing to go along with our questions, and just being really excellent guests. So I'd like to give you a big round of applause. Thank you.
[01:29:28.24] [APPLAUSE]
