Revolutionary plug-and-play CAR-T cell therapy could transform cancer immunotherapy
Researchers at the University of Chicago developed a “universal” chimeric antigen receptor (CAR) platform that offers enhanced safety, adaptability, and the potential to overcome long-standing barriers in cancer immunotherapy. Promising initial testing results, published in Science Advances, suggest that this new form of CAR-T cell therapy could dramatically change the treatment landscape for certain cancers.
Challenges with traditional CAR-T cell therapy
With CAR-T cell therapy, a patient’s own immune cells are harvested and genetically engineered to recognize a specific tumor antigen and attack cancer cells. Although CAR-T cell therapy has shown remarkable outcomes in certain blood cancers, it has struggled to succeed in solid tumors. The challenges include poor tumor penetration, toxic side effects, development of resistance mechanisms and the complex, patient-specific engineering process required for each treatment.
Traditional CAR-T cells rely on a fixed antigen-binding domain, which means they can only target one type of cancer antigen. A single CAR-T cell contains an antigen recognition unit attached to signaling machinery — making it a large construct that may contribute to toxicity. Moreover, tumors often display antigens in different degrees, and tumors may escape from CAR-T cell therapy by losing CAR-T targeted antigens.
A simpler and safer cell therapy approach
To address these limitations, UChicago researchers developed a new platform called GA1CAR. In this system, an engineered protein G variant (GA1) is fused to the T cell receptor signaling machinery, and the part that recognizes tumor targets is delivered in the form of short-lived antibody pieces known as Fab fragments.
These Fab fragments are engineered to specifically target the GA1 component on the surface of CAR-T cells, creating a strong yet reversible connection with a circulation lifespan of about two days. Without the Fab, GA1CAR-T cells stay inactive — unable to recognize or attack targets.
This modular “split” design separates the antigen-recognition element from the signaling machinery within the CAR-T cell, giving clinicians precise control over how, when, and where the engineered T cells attack cancer.
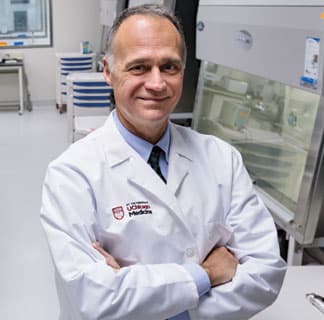
“This new CAR-T system acts like a plug-and-play device,” said co-lead author Anthony Kossiakoff, PhD, Otho S.A. Sprague Distinguished Service Professor of Biochemistry and Molecular Biology. “By simply switching the antibody fragment (Fab), we can redirect the same CAR-T cells to attack different cancer targets with greater safety and flexibility.”
One of the main limitations of traditional CAR-T cell therapy is toxicity. The GA1CAR system provides an “on-off” switch for enhanced safety.
“In our system, the targeting Fab has a short half-life — around two to three days in circulation — and if there’s a side effect, we can stop administering the Fab and essentially ‘pause’ the therapy without removing the CAR-T cells from the patient,” said Ainhoa Arina, PhD, Research Associate Professor in the laboratory of Ralph Weichselbaum, MD, Chair and Daniel K. Ludwig Distinguished Service Professor of Radiation and Cellular Oncology.
Multi-targeting and personalization approach
Beyond safety, the GA1CAR system’s flexible design offers rapid retargeting. Clinicians can administer one Fab to attack a specific tumor antigen and later switch to another Fab if the tumor evolves or develops resistance — without generating new CAR-T cells.
This flexibility is particularly valuable in solid tumors, where tumor heterogeneity — the presence of multiple antigens within the same tumor — has limited the effectiveness of single-target therapies.
In animal models of breast and ovarian cancer, GA1CAR-T cells were able to find and attack tumors by using different antibody pieces that target specific markers on cancer cells, such as HER2 and EFGR. These markers are often found in high amounts on certain cancer cells, so targeting them helps the T cells recognize and destroy the tumors more effectively.
“With this flexible system, we envision a future where a single CAR-T cell infusion can be reprogrammed with Fabs tailored to each patient’s tumor profile,” Arina said.
GA1CAR-T cells may be the way forward
In animal studies, GA1CAR-T cells performed the same as or better than conventional CAR-T cells and both therapies reduced tumor burden; however, GA1CAR-T cells showed greater activation and produced more inflammatory cytokines in response to the same antigen dose.
Importantly, GA1CAR-T cells maintained their function over extended periods and could be reactivated weeks later with a fresh dose of Fab. This capability opens the door for repeatable therapy where the dose can be adjusted as needed, without having to create new T cells each time.
Clinical implications and future plans
The research team is now exploring ways to integrate radiation therapy with the GA1CAR platform and to develop next-generation Fab fragments that stay in the body longer and reach tumors more effectively.
This study was a collaboration between the Department of Radiation and Cellular Oncology and the Department of Biochemistry and Molecular Biology at UChicago. Kossiakoff, an expert in protein engineering, developed the GA1 and Fab variants using phage display technology.
“Our lab handled the biochemical design and validation of the modular system,” Kossiakoff said. “Then we conducted in vivo testing in cancer models to prove that this strategy works beyond the test tube.”
With further refinements, the GA1CAR system could serve as a universal platform for precision immunotherapy — suitable for a wide range of cancers and potentially other diseases.
The study, “A universal chimeric-antigen receptor (CAR)- fragment antibody binder (FAB) split system for cancer immunotherapy,” was supported by Searle Foundation under the auspices of the Chicago Biomedical Consortium, the Ludwig Foundation for Cancer Research, and the National Cancer Institute.
Additional authors include Edwin Arauz, Elham Masoumi, Karolina Warzecha, Annika Saaf, Łukasz Widło, Tomasz Slezak, Aleksandra Zieminska, Karolina Dudek, Zachary Schaefer, Maria Lecka, and Svitlana Usatyuk from the University of Chicago.
Leaders in Cellular Therapy Care & Research
Cellular therapy — the transfer of human cells to heal or replace damaged tissue or cells — holds much promise for patients with cancer and other diseases. UChicago Medicine physicians are pioneers in cellular therapy care, including CAR T-cell therapy, stem cell transplantation and TIL therapy.
Learn more about cellular therapy at UChicago Medicine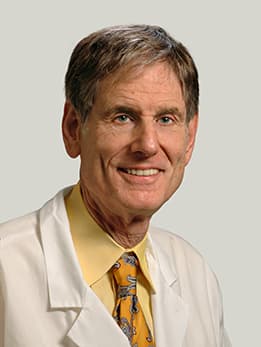
Ralph R. Weichselbaum, MD
Ralph R. Weichselbaum, MD, specializes in the potentially curative treatment of oligometastasis with radiation therapy. He serves as chair of the Department of Radiation and Cellular Oncology.
See Dr. Weichselbaum's profile