An innovative approach to classify metastases in patients with colorectal cancer
Once cancer spreads to different parts of the body (known as metastasis), it is more challenging to treat. This is true in colorectal cancer that has spread to the liver. However, some patients with limited metastasis can achieve long-term survival, and even a cure, if they're treated with aggressive localized interventions such as surgery or radiation therapy.
Now, University of Chicago Medicine Comprehensive Cancer Center researchers are using a new method they developed to accurately predict which patients with metastatic colorectal cancer will have a favorable treatment outcome (prognosis) following surgical removal of liver metastases. The method involves combining a panel of genetic biomarkers and clinical features of the tumor to determine distinct subgroups of cancer that correspond to different treatment outcomes. The findings were published in JAMA Oncology on July 20, 2023.
The new study builds on work published in oligometastasis” hypothesis, where cancer spread occurs along a continuum from a few to many sites.
An implication of the oligometastasis hypothesis is that cancers with limited spread in the body (typically one to five sites) can be eradicated with local interventions like surgery or radiation, while traditional palliative therapies like chemotherapy fail to eliminate metastatic disease.
“Over the past 30 years, the oligometastasis hypothesis has been supported by numerous clinical studies and revolutionized the treatment of metastatic disease,” said Pitroda. “Although curative therapies were shown to be promising, only 20% to 30% of patients with limited metastasis demonstrated long-term survival, indicating the critical need for biomarkers that could identify which patients derive the largest benefit from localized interventions, such as surgery.”
Discovery of molecular patterns
Prior to the latest study, UChicago researchers collaborated with colleagues at NorthShore University Health System, Evanston Hospital, to conduct a retrospective sequencing study from metastatic liver samples to identify molecular patterns underlying the differential patient outcomes. Based on messenger RNA (mRNA) and microRNA (miRNA) expression profiles, they found three distinct molecular patterns based on which metastases were categorized into canonical, immune, or stromal subtypes.
Among the three subtypes, the immune one exhibited the best prognosis. The tumor microenvironment in the immune subtype seemed to trigger an immune response in the liver, which might have helped to restrict new tumor growth and to achieve better treatment outcomes.
When molecular subtypes were combined with clinical factors, the authors derived three integrated risk groups which exhibited starkly different 10-year survival rates of 94%, 45%, and 19% for low-risk, intermediate-risk, and high-risk patients, respectively.
“Despite these promising results, we needed to validate our findings in an independent, prospectively collected clinical dataset before we can incorporate the three molecular subtypes into our clinical practice,” said Pitroda.
Validation of molecular subtypes
In the current study, researchers collected molecular profile data from 93 patients who had been treated at the University of Chicago Medical Center in Hyde Park. They derived an artificial intelligence neural network classifier to predict the molecular subtype of the disease. This group was considered a discovery cohort.
The team discovered 31 genes that predicted the molecular subtype with 96% accuracy. The neural network classifier was then applied to an independent group of 147 patients treated on the New-EPOC trial, who were called the validation cohort.
“When the molecular subtypes were combined with clinical features like tumor size and lymph node involvement, it strongly predicted the patient’s prognosis,” said Pitroda.
Patients with low-risk disease had an excellent chance of survival (80% at five years), in stark contrast to intermediate-risk (60% survival) and high-risk (40% survival) groups.
Significance of the work
The Ludwig Center for Metastasis Research at the University of Chicago is dedicated to understanding the biology of metastasis, and the current study serves the goal of this center, said Pitroda.
"We now have the first validated oligometastasis biomarker for predicting outcomes for patients with colorectal cancer spread to the liver. Our findings provide a novel framework for staging and classifying metastasis, which could lead to improved personalized therapy for patients by optimally integrating both local and systemic interventions,” said Pitroda.
We believe this will challenge the way we currently treat metastatic disease and open new opportunities to design future clinical trials and improve outcomes for our patients.
“Although we have conducted these studies in colorectal cancer metastasis, a similar approach could be applied to other types of cancer. We believe this will challenge the way we currently treat metastatic disease and open new opportunities to design future clinical trials and improve outcomes for our patients,” he added.
“Integrated clinical-molecular classification of colorectal liver metastases – A biomarker analysis of the phase 3 New EPOC randomized clinical trial” was supported by S:CORT (Stratification in Colorectal Cancer) and funded by grants from the Medical Research Council in Great Britain, Cancer Research UK, and the Ludwig Cancer Research Foundation.
Additional authors included Rohan Katipally, MD, Carlos Martinez, MD, Ralph Weichselbaum, MD, and Mitchell Posner, MD, from the University of Chicago Medicine; Sian Pugh, Addenbrooke’s Hospital, Cambridge, UK; John Bridgewater, MBBS, MRCP, PhD, University College London Hospital, John Primrose, MB, ChB, FRCS, MD, University of Southampton, UK; Enric Domingo, PhD, and Timothy S. Maughan, MD, University of Oxford, UK; Mark Talamonti, MD, NorthShore University Health System, Evanston, Illinois.

Sean P. Pitroda, MD
Sean P. Pitroda, MD, is an Assistant Professor of Radiation and Cellular Oncology at UChicago Medicine.
Learn more about Dr. Pitroda
Ralph R. Weichselbaum, MD
Ralph R. Weichselbaum, MD, specializes in the potentially curative treatment of oligometastasis with radiation therapy. He serves as chair of the Department of Radiation and Cellular Oncology.
See Dr. Weichselbaum's profile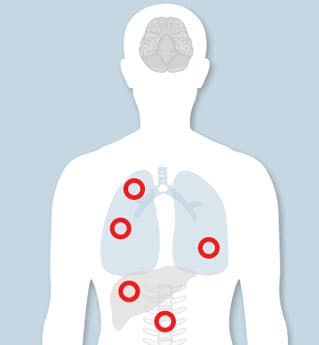
Treating Metastatic Cancer with Optimism and Hope
If you have been diagnosed with metastatic cancer, more therapies may be available to you than you think. Our cancer specialists are eager to help you understand all of your options.
Limited Metastatic Cancer Program