Debunking six myths about multiple sclerosis
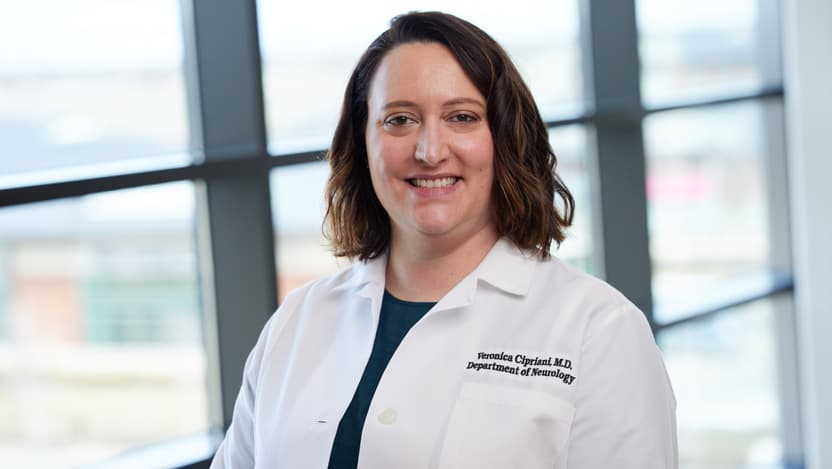
Veronica Cipriani, MD, is a neurologist who specializes in the diagnosis and treatment of multiple sclerosis.
University of Chicago Medicine specializes in treating multiple sclerosis (MS), an autoimmune disease in which the myelin sheath around nerve cells is stripped away and, depending on where these nerve cells are located, causes neurological symptoms such as numbness, weakness or loss of vision, to name a few.
As a neurologist who specializes in the diagnosis and treatment of MS, I often speak with patients to clear up misinformation about the disease. Here are six myths that persist about MS.
Myth: Multiple sclerosis only affects young, white women.
People of most ethnicities are affected by MS, including Black people, Latinos and Asians — not just young, white women, although white people of Northern European ancestry are at an increased risk for MS. The most recent statistics show 1 million people in the U.S. are living with MS.
We do, however, know that MS is three times more common in women than men, even though men tend to have more aggressive or disabling MS. MS may also be more aggressive or disabling in people with different races and ethnicities. There have been studies over the years about whether taking hormones such as estradiol, the strongest type of estrogen in the body, reduces the relapse rate of MS. To date, none of these hormone treatments have panned out.
Myth: Multiple sclerosis does not affect African Americans.
Not only can Black Americans develop MS, but studies suggest the highest incidence of MS is in Black American women. This knowledge should definitely make us think about inclusion — MS clinical trials of disease-modifying medications have traditionally involved fewer than 10% of Black participants. Even though the rate of MS is high in Black Americans, they’re not being sufficiently recruited into clinical trials, and we’re essentially extrapolating that medications work just as well in this group as for others. We’re working to change that, however, by promoting awareness of this disparity and calling for more equity in clinical trial research to come.
Myth: People with multiple sclerosis have a much more difficult time getting pregnant and having children.
It used to be said that fertility decreased with MS, but we now know that’s not true. People with MS get pregnant and even have unplanned pregnancies. Ideally, patients should discuss with their doctor before getting pregnant because some MS medications aren’t recommended for use during pregnancy. You may need to pause or change your medications during pregnancy and for a period of time after giving birth.
Myth: Multiple sclerosis is not affected by pregnancy and menopause.
Pregnancy tends to protect MS patients from flares, especially in the second and third trimester. It’s believed this is due to changes in the immune system caused by hormones. This generally lasts up to three months after pregnancy, so having an appointment soon after giving birth to discuss a plan for getting back on your medications is important.
After menopause, MS can become more progressive than relapsing. The changes in hormones may make MS symptoms worse, including by causing hot flashes.
Myth: Patients with multiple sclerosis can’t breastfeed.
Breastfeeding is incredibly beneficial for your baby, and there’s no way your baby can ‘catch’ MS through breast milk. Research also suggests that exclusive breastfeeding may actually reduce your chance of relapsing. But the likelihood of having a flare-up increases in the weeks after giving birth, so it’s important to see your doctor during that period to discuss your plan for breastfeeding and what medications may be used during breastfeeding. Not all of them are safe because they can pass through the breast milk to your baby.
Myth: If you have multiple sclerosis, then your children will have multiple sclerosis, too.
Most children with a parent or parents who have MS will not develop MS later in life — but those children are at an increased risk for developing it. We still don’t fully understand what causes MS. It does have a genetic component, but there are many other environmental factors that play a role, including age, sex, Epstein-Barr virus exposure and vitamin D deficiency.

Veronica Cipriani, MD
Veronica Cipriani, MD, is a neuroimmunologist who specializes in the treatment of multiple sclerosis and other demyelinating neurologic diseases such as neuromyelitis optica and anti-MOG encephalomyelitis.
Learn more about Dr. CiprianiSchedule a Multiple Sclerosis Appointment
Schedule an Appointment Online
Schedule an appointment instantly with one of our Multiple Sclerosis experts through our online scheduling portal.

Second Opinions at UChicago Medicine
We welcome patients who seek second opinions for MS, and offer both on-site and remote second opinions. Our experts can confirm your diagnosis and recommend a treatment plan that’s best for you.
