What is an abdominal aortic aneurysm (AAA) and what are the symptoms?
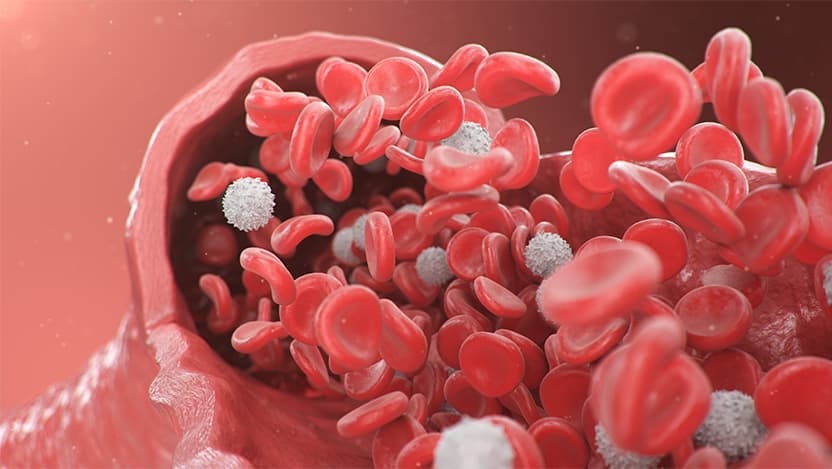
The abdominal aorta is the main blood vessel supplying blood to the abdomen, pelvis, and legs. When this vessel enlarges, forming an aneurysm, it can be life-threatening. Knowing who is at risk and screening early is crucial to prevent a deadly rupture.
What is abdominal aortic aneurysm (AAA)?
An abdominal aortic aneurysm occurs when a portion of the aorta enlarges. Normally, the abdominal aorta is a round, pipe-like structure about the size of a golf ball. An aneurysm causes the aorta to expand, weakening its walls and increasing the risk of a potentially fatal burst.
Common Causes of Abdominal Aortic Aneurysm
Research has identified key risk factors for developing AAA, including:
- High blood pressure (especially poorly controlled high blood pressure)
- High cholesterol
- Smoking
Family history also significantly impacts risk. If multiple family members have had AAAs, the likelihood increases for having an aneurysm, but it does not guarantee that other family members will develop aneurysms.
Abdominal Aortic Aneurysm Symptoms
Detecting an AAA before you feel symptoms would be best because symptoms typically suggest that the aneurysm is under significant pressure and at high risk of rupturing. The easiest way (and best time) to find the aneurysm is with a basic physical examination while you are asymptomatic (not experiencing any typical symptoms), but we can detect an aneurysm with a screening test if needed.
AAA Screening: Ultrasound
Detecting an AAA before you feel symptoms would be best because symptoms typically suggest that the aneurysm is under significant pressure and at high risk of rupturing. The easiest way (and best time) to find the aneurysm is with a basic physical examination while you are asymptomatic (not experiencing any typical symptoms), but we can detect an aneurysm with a screening test if needed.
AAA Screening Guidelines
If you have a family history of AAA, you should start getting screened at age 50. If your first screen is normal, I usually recommend you get checked again in 10 years. I really stress with my patients that they should let family members know how important it is that they get screened as well. I've had a number of brothers and sisters, as well as children, come in to get screened. We have been really diligent about promoting the screenings to family members of patients with family history, encouraging a follow-up evaluation.
If you do not have a family history but do have AAA risk factors (high blood pressure, high cholesterol, smoking), we suggest you begin screening at age 65. If you have a normal screening, it is likely that you will never have to be checked again. However, if your scan shows that an enlarged aorta, we will recommend rechecking once a year, or every other year, until the AAA grows to a size where we need to check it more frequently.
Abdominal Aortic Aneurysm Treatments
We usually repair the aorta when an aneurysm reaches about 5 or 5.5 centimeters in width.
There are two general approaches we can take to repair aneurysms. One is with a standard, open abdominal surgery that has been done for many years. Open surgery is successful in repairing the aneurysm, however is a much more intensive procedure. This technique is often used for more complex patients who require standard surgical methods because their aorta needs to be shaped properly in order to be successful.
The second approach has been developed more recently over the past two decades. It's an endovascular (or stent) technique in which the aneurysm is repaired in a much less with a minimally invasive procedure. A lot of. Many aneurysms can now be treated with an endovascular procedure and about 90 percent of the patients we see at UChicago Medicine are able to have their aneurysm fixed with stents.
Survival Rate and Recurrence of AAA
The survival rate post-surgery is generally very good. While rare, there is a slight risk of developing another aneurysm either in a different part of the aorta or experiencing issues with the original repair. Regular follow-ups, typically annually or biannually, are conducted to monitor for any new heart problems.
Why choose UChicago Medicine for AAA treatment?
UChicago Medicine's Center for Aortic Diseases is internationally known for aortic care, and offers a comprehensive, multidisciplinary approach. The team includes anesthesiologists, cardiologists, surgeons, ICU teams and nurses, providing a wide range of treatment options tailored to each patient.
Future of Abdominal Aortic Aneurysm Treatments
In medicine, we are always looking for ways to improve care for our patients. Right now, we are using new techniques that enable us to treat more of the aorta with endovascular, or less invasive, approaches. Because UChicago Medicine is on the leading edge of medicine, we're involved in various clinical trials that provide us access to devices sooner than other medical centers. We're able to treat more complicated aneurysms, and different parts of the aorta, with less invasive techniques.

Ross Milner, MD
Ross Milner, MD, is an internationally recognized expert in vascular surgery. He specializes in the treatment of complex aortic diseases.
Learn more about Dr. Milner
Center for Aortic Diseases
For over 100 years, the world-renowned clinicians and scientists at the University of Chicago Medicine have specialized in the diagnosis, care and management of all types of aortic conditions.
Explore our aortic disease servicesRequest an Appointment
We are currently experiencing a high volume of inquiries, leading to delayed response times. For faster assistance, please call 1-773-702-6128 to schedule your appointment.
If you have symptoms of an urgent nature, please call your doctor or go to the emergency room immediately.
* Indicates required field
