Clinical trials look to improve surgery for frail patients
After 18 months of data collection, a group of University of Chicago Medicine physicians and scientists will expand their ongoing lung cancer clinical trial to include collaboration from the University of Michigan in Ann Arbor this April.
The UChicago Medicine team, led by Mark Ferguson, MD, has been conducting research on how frailty can adversely affect patient outcomes following complex surgery, including lung cancer resection, or surgical removal of all or part of the lung.
What started with a philanthropic gift from Jeanie Dallas, one of Ferguson's patients, has turned into multiple clinical trials with more than 150 participating patients--and growing.
Science Life spoke with Ferguson to learn more about the research, and what his team hopes to do next.
What has your initial research found regarding patient frailty and surgery?
So far we've screened 150 patients prior to major surgery, with the majority being lung resection patients. We've found 70 percent of them to be frail or pre-frail – 55 percent pre-frail and 15 percent frail. Falling into one of these two categories puts them at risk for complications after surgery, including prolonged recovery times and the potential need to recover in a nursing or rehab facility. These patients are also at a higher risk for readmission, they suffer from lower quality of life following surgery, and they end up paying higher overall costs for their care.
How is your team attempting to change the frailty status of these patients?
In the short-term, we put them on an exercise regimen to build strength and endurance. We've designed a frailty intervention trial, which opened in August 2015, that includes providing at-risk patients with a complete geriatric assessment of their physical status, nutrition, medications, mood and environmental factors – anything that may put them at risk for adverse outcomes.
The exercise regimen focuses on improving endurance, strength and balance through a combination of supervised physical therapy and at-home work. The program is designed to last six weeks, a time interval we do not believe negatively impacts the outcomes of cancer treatment.
How is data collected?
For the study, we have the patients fill out a daily diary for activity, and wear wrist, ankle and waist devices to measure aspects of the activity. Later in the trial, we will sort through the collected data to verify their activity and see how it correlates with outcomes after surgery.
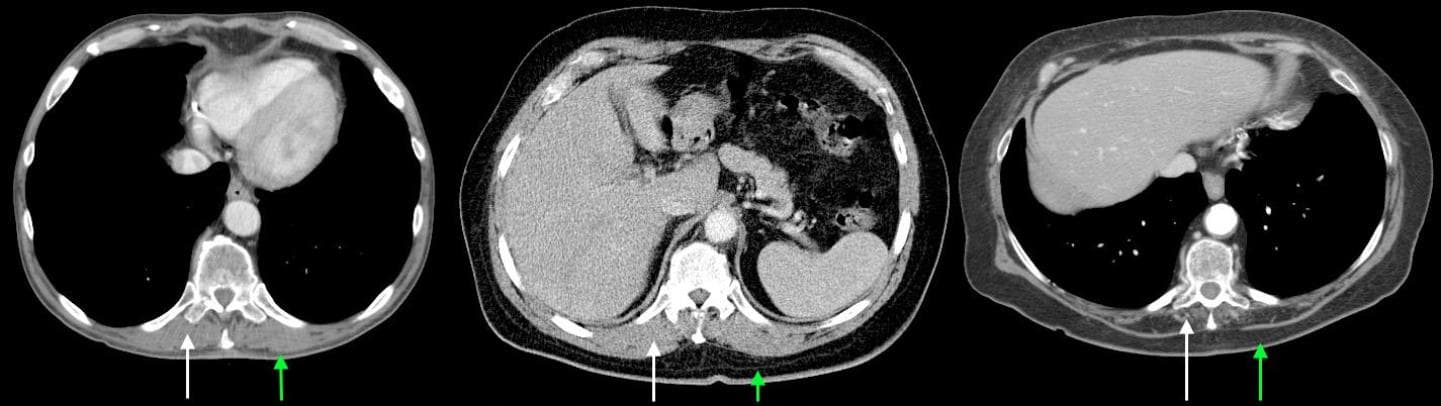
In conjunction with colleagues at the University of Michigan, we are also measuring patients' core muscle mass on a standard CT scan, since low muscle mass likely correlates with frailty. We recently found that patients with a low BMI are at increased risk for postoperative complications after lung resection, and these patients are also more likely to be frail.
Most surgeons don't recognize frailty as an entity. It's easier to perform an operation on a thin person than an obese person, but an underweight patient is actually at a much higher risk for problems than a person with a normal to high BMI. Fortunately, frailty recognition can easily be taught and the importance of this factor in assessing risk is increasingly recognized. With such efforts we are trying to get away from an instinctual approach to assessing patients by creating a more structured approach, much like the automated pain score.
What is your overarching goal?
Some physicians, including myself, have intuitively been using frailty indicators to assess patients for decades. However, without clear mechanisms in place, the screenings have never been standardized. Also, without compelling outcomes data for the benefits of exercise, it's hard to motivate patients and to help them understand how worthwhile these relatively simple interventions can be. Once we complete this study, we believe the data will be convincing – for patients and physicians – that frailty is a problem and one that we can tackle successfully to improve patient outcomes and overall wellbeing.
What are the next steps for this project?
Our clinical trial began in August, and we have approval for 18 months. After that, we hope to continue it on a year-by-year basis, depending on the availability of funding.
The current frailty interest group at the University of Chicago is comprised of experts in geriatrics, physical therapy, nutrition, respiratory and muscle metabolism, and surgery. In addition to frailty screening and exercise interventions, we are beginning to look at molecular processes that are correlated with weakness and low muscle mass. These findings will be correlated with muscle mass/density measurements from CT scans. Identifying these mechanisms may help us develop personalized treatments.
This is an incredibly collaborative effort – we have a big team of people working on these trials. In April, we will have our first working group meeting with clinicians, basic scientists, and colleagues from the University of Michigan. Science depends on a large number of dedicated people working together. Read more from Science Life about the trial's beginnings.
