What you need to know about peripheral artery disease
What is peripheral artery disease?
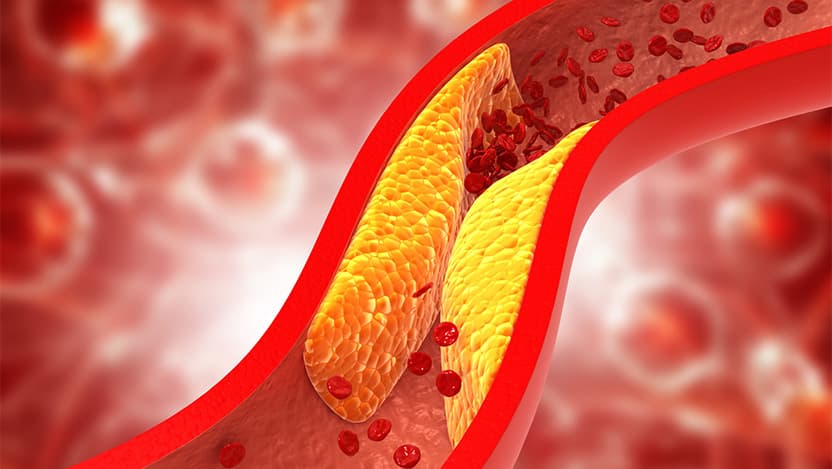
Peripheral Artery Disease (PAD) is a condition where the arteries that carry blood away from the heart become narrowed or blocked by a buildup of plaque. The reduced blood flow can result in pain in your legs, feet and toes.
The most common symptom is claudication – pain while walking, a discomfort that goes away with rest. However, some people with PAD develop a severe blockage called critical limb ischemia, which can lead to gangrene and amputation if untreated.
PAD often goes undiagnosed, so it’s important to talk with your doctor if you’re having symptoms. By starting treatment early, you can stop the disease from progressing and avoid potential complications, including amputation.
As a vascular surgeon at UChicago Medicine, I treat patients with PAD and help determine the best course of treatment to reduce their risk and improve their quality of life.
What are some factors that can increase risk for PAD?
The most important risk factor is smoking. Any current or former smoker is at very high risk for developing PAD. Certain medical conditions also increase risk, including high cholesterol, diabetes, and high blood pressure. If you have diabetes, talk with your doctor about getting regular screening for PAD.
How can people reduce their risk of PAD?
I can't emphasize enough the importance of stopping smoking. Smoking cessation, and managing additional risk factors (like cholesterol, blood pressure, and diabetes) are the main ways to reduce the risk of developing PAD. If you have PAD, talk with your doctor about reducing the risk of additional complications. That could include making sure that you're taking the proper medications, such as an antiplatelet medication like aspirin as well as cholesterol-lowering medications like statins. We encourage all our PAD patients to exercise regularly, working up to a daily 30-minute walk.
Does PAD increase risk of other diseases?
PAD is a form of atherosclerosis (the buildup of plaque in the blood vessels). People with atherosclerosis in one part of their body generally have it throughout their entire body. So if you have PAD, you're also at risk for heart disease, stroke, and cerebrovascular disease.
What are warning signs that should lead someone to see their doctor about PAD?
The three most important warning signs: pain while walking that's relieved by rest; a sore or wound on the foot or toes that is slow to heal; and significant foot pain at night, especially if the pain goes away when you hang your foot over the bed. If you have any of these symptoms, you should see your physician.
How is PAD treated?
When the main main symptom is pain while walking, we start with nonoperative medical management, which means controlling the PAD through medication and avoiding surgery. That involves lifestyle changes like exercise, and making a really strong effort at smoking cessation. The vast majority of patients who comply have low rates of complications. They also see their walking distance improve to the point that PAD stops being a lifestyle-limiting condition.
For patients with the more severe form of the disease, critical limb ischemia, we do additional testing to determine the next best treatment option. This may be a minimally invasive intervention like an angiogram, or, if the condition is more severe, bypass surgery to reroute blood flow around the blockage.
What should people know about atherectomy as a treatment for PAD?
Atherectomy is a surgical procedure that involves cutting away away plaque. We don’t do atherectomy as a treatment for PAD at the University of Chicago Medicine because of some of the issues raised with the procedure. While the goal is to open the arteries, studies have shown that this procedure can increase risk of amputations. It is also unnecessary for the vast majority of patients with PAD. Patients whose main symptom is pain with walking are best served with nonoperative medical therapies. Asymptomatic patients may not need treatment at all. If your provider is really pushing surgery or other interventions, it's always a good idea to get a second opinion from a vascular surgeon.
Is it safe to take aspirin for PAD?
There has been a lot of press about the dangers of taking aspirin every day. That may be true for the general population, but for patients who have peripheral artery disease, it's really important that they take the medications –including aspirin – as prescribed by their physicians. If there are any concerns about taking those specific medications, make sure you talk to your doctors. But medications including aspirin are crucial. We have no ability to cure PAD or cause plaque to regress, but we can stop the progression of the disease with medication.
What else can people do to improve their outcome?
It's always best to seek treatment early. There's a lot of fear in our patient population, because many people have had friends or family members who have undergone amputation. Sometimes people don't want to seek treatment, because they are afraid of what the outcome is going to be. But frequently, we can achieve better outcomes if we're involved earlier in the disease process. So anytime there's a warning sign, especially if you have diabetes or another condition that puts you at high risk, make sure you speak to your doctor right away.

Trissa Babrowski, MD
Trissa Babrowski, MD, is an expert in vascular surgery. Dr. Babrowski specializes in the treatment and management of complex vascular and aortic conditions, with a primary focus on limb salvage.
Learn more about Dr. BabrowskiPeripheral Artery Disease (PAD)
University of Chicago Medicine's PAD team is uniquely positioned in the community to provide advanced treatment for patients who have a higher risk of developing peripheral arterial disease.
Learn more about peripheral artery disease.