Targeting metabolic and inflammatory pathways suppresses tumor growth in pancreatic cancer
Pancreatic cancer (PC) is one of the most aggressive, hard-to-treat types of solid tumor cancer. Because of its poor prognosis and resistance to current therapies, PC is expected to become the second-most common cause of cancer-related deaths by 2030.
Despite extensive research to understand PC tumor biology, effective therapies are lacking. Recently, researchers at the University of Chicago Medicine and their colleagues from the Sloan Kettering Institute uncovered key insights into why normal cells turn into tumor growth-promoting cells.
This process involves a condition called hypoxia, where different types of cells found in a tumor become oxygen-starved and stimulate cancer cells to release small proteins called cytokines. In a mouse model of pancreatic cancer, the researchers noticed these two factors play a key role in converting normal cells in tumors into inflammatory cells that accelerate tumor growth.
“By blocking hypoxia, or its downstream effects in the normal cells, it is possible to control tumor growth and potentially make advanced therapies like immunotherapies work in pancreatic cancers,” said Simon Schwörer, PhD, first and co-corresponding author of the paper who is an Assistant Professor of Medicine at the University of Chicago Medicine Comprehensive Cancer Center. The study was reported May 15, 2023 in Cancer Research, a journal of the American Association for Cancer Research.
Cellular makeup of tumor tissue
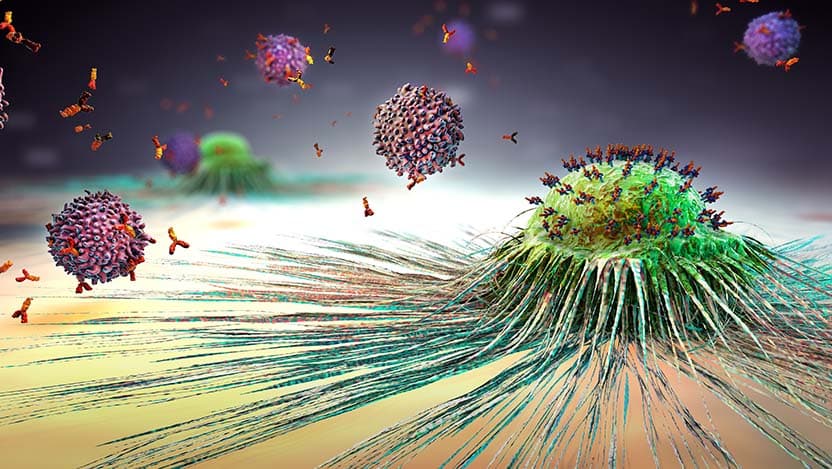
The work of Schwörer and colleagues focuses on a branch of oncology research called cancer metabolism, which studies how cancer cells utilize nutrients to survive and grow. A major contributor to tumor growth is the tumor microenvironment (TME), which consists of a variety of components, including blood vessels, immune cells, fibroblasts, signaling molecules, and the connective tissue called extracellular matrix (ECM).
The fibroblasts and the ECM hinder nutrient supply to the tumor and also cause resistance to treatment. Earlier studies have hypothesized that tumor growth can be controlled by removing the fibroblasts. However, the opposite was true. When the fibroblasts were removed, tumor growth escalated.
“Research studies have identified that there is a heterogeneity – in other words, a variety – of fibroblast cells in tumor tissue, with some cells promoting and others inhibiting tumor growth,” said Schwörer. “It is important, therefore, to identify the ones that promote tumor growth and only target those to control tumor progression. To do so, we need to understand how these cells work.”
Hypoxia in promoting tumor growth
As cancer progresses, the growth of the tumors overtakes the oxygen supply provided by blood vessels. This creates a hypoxic environment that can affect the cancer cells themselves as well as the other cells in the TME.
In the current study, Schwörer and colleagues found that tumor hypoxia in pancreatic cancer can convert normal fibroblasts into tumor-promoting inflammatory fibroblasts, also called cancer-associated fibroblasts (CAFs). Inflammatory CAFs (iCAFs) produced in tumor tissue due to hypoxia release a variety of growth factors and inflammatory cytokines that drive tumor progression.
The next question was whether hypoxia alone produces iCAFs or if other existing conditions in the TME combine with hypoxia in tumors to promote the production of iCAFs.
In the current study, researchers observed that the cancer cells in pancreatic tumor tissue produce inflammatory cytokines. When hypoxia factors into this condition, it enhances the effects of inflammatory cytokines, switching fibroblasts from normal to an inflammatory state. Both the inflammatory condition and metabolic state of hypoxia collude to promote tumor growth.
According to Schwörer, the team was able to reduce the growth of tumors in animal models by blocking the hypoxic signals in the fibroblasts.
"This study shows that the metabolic features of the tumor microenvironment can orchestrate functional diversity in CAFs and identifies hypoxia as a master regulator of inflammatory CAFs and tumor growth in pancreatic cancer,” Schwörer concluded.
Regulating tumor environment to prevent tumor growth
Hypoxia not only enhances the ability of cancer cell-secreted cytokines to convert normal fibroblasts into inflammatory fibroblasts. These hypoxic, inflammatory fibroblasts also promote tumor growth.
This effect seemed unassociated with direct interaction with the cancer cells. Now, researchers are interested in understanding how the hypoxia-educated fibroblasts communicate with and potentially affect other cells in tumors – such as endothelial and immune cells –to promote pancreatic tumor growth.
“Understanding the role of hypoxia in generating inflammatory fibroblasts and their interactions with immune system will provide some insights towards the resistance to immunotherapy in pancreatic cancer,” Schwörer said. “Also, studying the nutrient environment and tumor metabolism and how they regulate tumor heterogeneity is critical in understanding the really complex tumors like pancreatic cancer.”
The study, “Hypoxia potentiates the inflammatory fibroblast phenotype promoted by pancreatic cancer cell-derived cytokines,” was supported by the National Cancer Institute, the AGA Research Foundation, the Hirshberg Foundation, an ACS-IRG Pilot Grant, the Sandra Gerry Metastasis and Tumor Ecosystems Center at Memorial Sloan Kettering Cancer Center, the Memorial Sloan Kettering Cancer Center's (MSKCC's) David Rubenstein Center for Pancreatic Research Pilot Project, and an MSKCC support grant.
Additional authors include Francesco V. Cimino, Kaloyan Tsanov, PhD, Charles Ng, MD, PhD, Craig B. Thompson, MD, from Memorial Sloan Kettering Cancer Center, New York; Manon Ros, PhD, Carlos Carmona-Fontaine, PhD, from New York University, New York; Scott Lowe, PhD, from Memorial Sloan Kettering Cancer Center, New York, and the Howard Hughes Medical Institute in Chevy Chase, Maryland.

UChicago Medicine Comprehensive Cancer Center
UChicago Medicine is designated as a Comprehensive Cancer Center by the National Cancer Institute, the most prestigious recognition possible for a cancer institution. We have more than 200 physicians and scientists dedicated to defeating cancer.
Learn More About the Comprehensive Cancer Center