How T cells learn when to wield their special immunological weapons
T cells — a major weapon of the adaptive immune system — are crucial for orchestrating immune responses against pathogens and cancer cells. Much of the DNA configuration important for their ability to fight invaders happens before the cell fully becomes a T cell.
Transcription factors, a group of proteins that bind to DNA sequences to determine a cell’s fate, work together with large molecular motors called chromatin remodeling complexes to open regions of the genome important for T cell function early in development. According to new research from the University of Chicago, this lets the T cell activate the appropriate genes when they encounter their target antigens.
How do T cells activate their specialized functions?
T cells can control activities of other immune cells or directly kill target cells to keep the host organism safe and healthy. But how T cells know when to activate specific immune functions when they recognize harmful entities has been a longstanding question in the field.
Andrew Koh, PhD, Assistant Professor in the Department of Pathology at the University of Chicago, and his team conducted a study to understand how T cells integrate what they sense in the external environment with their internal machinery to generate the right responses to help eliminate pathogens or cancers. The results were published in Nature Immunology on April 17, 2024.
“A particularly puzzling aspect of this question is that the specialized sensing apparatus that T cells use to recognize foreign entities triggers the same signaling pathways that activate entirely different functions in other cell types,” Koh said. “Instead of the sensing apparatus determining how a T cell responds, we wondered whether the key is in how the T-cell genome is prepared in development prior to encountering its target antigen.”
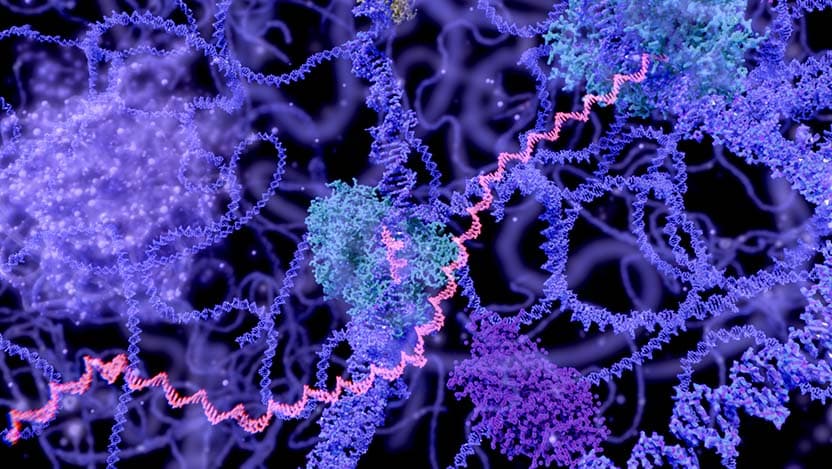
Signaling pathways are a chain of molecular events that activate a cell’s genes. Transcription factors are activated by molecules sensed outside of the cell and then enter the nucleus and find target genes. At any given time, these signal-responsive transcription factors bind to only a small fraction of the total binding sites across the genome. This is because DNA is largely arranged in a condensed form, wrapped around histone proteins — called chromatin — that act as barriers.
Each cell type has a unique chromatin configuration, and only a subset of the DNA that encodes the relevant functions is accessible. Koh and colleagues asked when and how the chromatin configuration specific to T-cell functions becomes established during T-cell development.
“We were very surprised to find that a substantial fraction of the chromatin landscape specific to activated T cells is established at the very first stage of T-cell development, prior to the expression of the antigen receptor,” Koh said. “So, it appears the cells know to some degree what they will need when they encounter pathogens or cancer much further down in the maturation process.”
Keeping the genome open at the right time
Koh and colleagues next sought to determine how the T cell prepares the genome early in development. They found that this process depends on a particular chromatin remodeling complex called mSWI/SNF (or BAF) that opens regions of the genome that were previously compact and inaccessible. But the BAF chromatin remodeling complex doesn’t bind specifically to any particular DNA sequence, thus it doesn’t know which regions of the genome to open up.
“So, the next major goal of the project was to identify transcription factors that partner with BAF to open up the regions that the T cells need in the future,” said Noah Gamble, a graduate student in Koh’s lab, and first author of the paper.
The researchers found that during the first stages of T-cell development, transcription factors named PU.1 and RUNX1 work together to recruit BAF to the regions of the genome that encode T-cell function. However, the transcription factor network soon changes as the cell develops to fully commit to becoming a T cell. PU.1 is no longer expressed by the third stage of T-cell development and RUNX1 is left needing a partner to keep BAF recruited to the appropriate regions of the genome. As PU.1 expression is extinguished, another transcription factor, BCL11B, is expressed and partners with RUNX1 to maintain accessibility at the regions encoding T-cell functions.
“There’s a relay that happens where BAF is handed off from one set of transcription factors to another to ensure that these regions of the genome stay open throughout development, so that when the T cell finally matures and encounters pathogens or cancers, it will elicit T-cell-specific responses and not B cell-specific responses or something else,” Koh said.
How developing T cells know when to stay active
For the system to work, the regions of the genome encoding T-cell functions have to be open, but they can’t be activated until the T cell recognizes its target antigen. There is a fine balance between the positive forces that open these regions and the repressive forces that prevent them from turning on too early. Koh plans to focus future research on identifying the negative regulators that could be involved in maintaining this precarious balance.
Understanding how chromatin is configured in specific ways could also potentially allow synthetic manipulation of its landscape to control what T cells do in response to specific disease contexts.
“The dream is to take out T cells from a given patient that's fighting a particular disease, manipulate the chromatin landscape in a way that skews the T cells towards a particular function, and return the engineered T cells back to the patient to facilitate a more efficacious immune response,” Koh said.
The study ‘PU.1 and BCL11B sequentially cooperate with RUNX1 to anchor mSWI/SNF to poise the T cell effector landscape’ was funded by the National Institute of Health (NIH)/National Institute of General Medical Sciences (NIGMS). Noah Gamble was supported by NIH T32 training grants and the Robert E. Priest Fellowship.
Additional authors include Alexandra Bradu, Jason Caldwell, Joshua McKeever, Olubusayo Bolonduro, Ebru Ermis, and Caroline Kaiser from the University of Chicago and YeEun Kim, Benjamin Parks, Sandy Klemm, William Greenleaf, and Gerald Crabtree from Stanford University, CA.

CAR T-Cell Therapy
CAR T-cell therapy supercharges a patient's white blood cells to find and destroy cancer cells. UChicago Medicine research played a key role in the development of this exciting new immunotherapy.
View videos and learn more