Our Vascular & Interventional Radiology Team
At The Forefront Live: Prostate Health and Treatment Options
At The Forefront Live: Prostate Health and Treatment Options
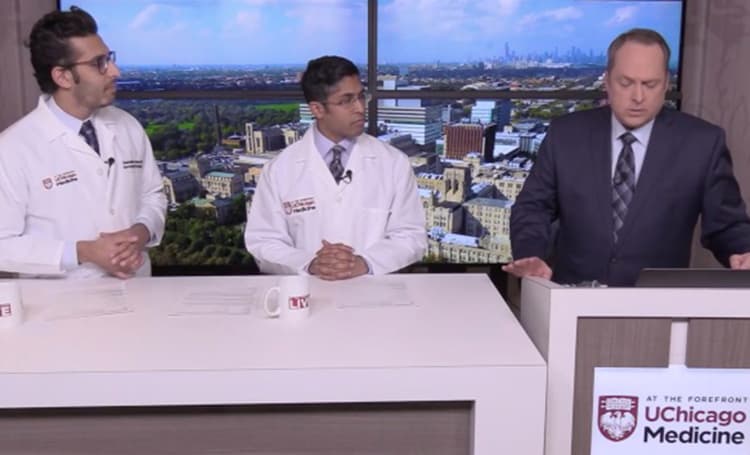
We spoke with experts Rakesh Navuluri, MD, and Osmanuddin Ahmed, MD, about benign prostatic hyperplasia (BPH) and the non-invasive treatment options available at UChicago Medicine.
