Ready-to-go T cells may be responsible for immunotherapy success in classical Hodgkin lymphoma
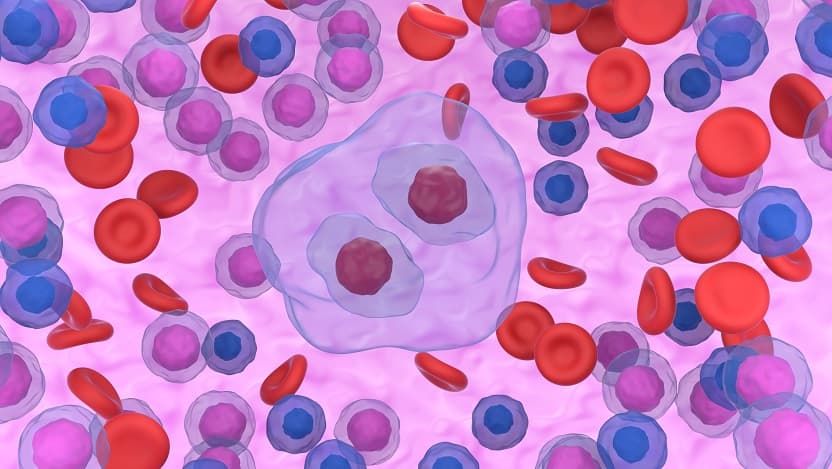
The presence of large white blood cells with multiple nuclei, called Reed-Sternberg cells (pictured), are a hallmark of Hodgkin lymphoma.
Researchers from the University of Chicago Medicine Comprehensive Cancer Center described how T cells with specific tasks join forces against classical Hodgkin lymphoma (cHL) in a study published in Cancer Immunology Research. Their insights could advance immunotherapy as an effective treatment for cHL.
This rare cancer of the immune system primarily affects adults in their 20s and 30s. Patients respond well to immunotherapies like immune checkpoint blockades (ICBs) and the anti-PD-1 drug pembrolizumab (Keytruda), thought to work by “taking off the brakes” of the immune system to let it kill tumor cells.
Currently, cHL has an 89% five-year survival rate based on these existing therapies. Ongoing research is trying to understand why cHL is much more responsive to ICBs than other tumor types. The answer may help researchers develop strategic, immunotherapy-based treatments that enhance effectiveness in other cancers.
A focus on T cells in cHL
T cells have many different functions. CD8+ “killer” T cells, as their name suggests, can kill infected or cancerous cells. CD4+ “helper” T cells coordinate the immune response by assisting CD8+ T cells or antibody-producing B-cells.
Regulatory T cells are important in helping to control immune responses, often by suppressing other immune cells. All these types of T cells are present in cHL tumors.
Study author Xiufen Chen, PhD, a research scientist at UChicago, describes cHL as a unique lymphoma. “The cancer cells actually only make up 1% to 2% of the whole tumor,” she said. Most cells in the tumor are noncancerous immune cells, including numerous T cells that surround the cancer cells.
Previous work from British Columbia Cancer revealed that CD4+ “helper” T cells and regulatory T cells play a key role in the tumor microenvironment of cHL, which includes both cancer cells and the cells nearby. Chen and Justin Kline, MD, Professor of Medicine and director of the lymphoma program at the University of Chicago Medicine, expanded on the characterization of the cHL tumor by combining single-cell sequencing with T-cell receptor (TCR) sequencing and functional experiments to test the responses of T cells from the tumor.
They collected biopsy samples from 14 patients with cHL and five patients with noncancerous reactive lymphoid tissue (RLT). Using single-cell sequencing or functional analysis to process portions of these samples, the researchers found that cHL was dominated by CD4+ and regulatory T cells compared to RLT samples. Researchers also observed that both effector CD8+ and exhausted CD8+ T cells were present in the cHL samples.
This difference in phenotype of CD8+ T cells is important, Kline explained. “CD8+ cells that repeatedly encounter tumor antigen in situ initially demonstrate effector function. They kill and they secrete cytokines, but then they get a little bit worn out and lose that function.”
CD8+ T cells are expanded and functional
Chen and colleagues hypothesized that TCR sequencing can indicate whether T cells are diverse or expanded copies from a single original cell. An overlap of TCRs suggests that the T cells specifically target cancer cells.
Most shared TCRs were exhausted or effector CD8+ T cells in cHL, suggesting the “killer” T cells recognized cHL cancer cells. The cHL samples also showed some expansion of regulatory T cells, which could suppress a local immune response. Though CD4+ T cells are the most abundant in the tumor, the researchers saw little to no clonal expansion of CD4+ cells.
Chen used flow cytometry to measure expression of inhibitory markers, such as the common ICB target PD-1. Therapies targeting PD-1 are commonly used as part of first-line treatment because of their effectiveness in cHL.
In cHL samples, CD8+ T cells were more likely to express inhibitory markers. CD4+ T cells were less likely to express inhibitory markers when compared to RLT tumors. While inhibitory markers can suggest CD8+ T cell exhaustion, they were rare, making up about 6% of the cells in the tumor.
When T cells from cHL were restimulated, they were able to express important functional proteins, such as pro-inflammatory cytokines and granzyme, at higher levels than T cells from RLT. Based on these results, researchers said, it is unlikely that cHL induces deep exhaustion or dysfunction of T cells in the tumor.
“It’s almost like these T cells are poised. They’re not terminally exhausted, they still have function, but they are being restrained by the strong expression of PD-L1 by the lymphoma cells,” Kline said.
Kline hopes this study generates interest, as it challenges the role of various T cells in cHL. Yet he emphasized that many questions remain unanswered. “I think it’s possible that we may never know why anti-PD-1 therapy is so effective in Hodgkin lymphoma," he said.
Additional authors of the study, “T-cell States, Repertoire, and Function in Classical Hodgkin Lymphoma Revealed through Single-Cell Analyses,” include Jovian Yu, Girish Venkataraman, Sonali Smith, Mengjie Chen, Alan Cooper, Sravya Tumuluru, and James Godfrey from the University of Chicago. Author Joshua Brody is from the Icahn School of Medicine at Mount Sinai.

Justin Kline, MD
Justin Kline, MD, is a hematologist/oncologist who specializes in treating leukemia and lymphoma. He has a special interest in stem cell transplantation and is conducting research into overcoming the barriers to immune resistance mechanisms in tumors.
See Dr. Kline's profile