Understanding seizure mapping and laser ablation surgery
If your seizures cannot be controlled with medications, then you may be a candidate for surgery to help you achieve seizure freedom.
UChicago Medicine’s neurosciences teams are some of the most experienced in the country for the diagnosis and treatment of epilepsy, and our neurosurgeons have implanted more than 300 laser fibers to surgically treat seizures. Our care team members will support you each step of the way to identify, treat and effectively manage your seizures.
Finding the seizure focus
First, our team of neurologists and neurosurgeons will use data from different brain maps to identify the exact focus – or starting point – of your seizures prior to surgery. We use different types of brain maps to identify precisely where your seizures are originating. Finding the seizure source — or seizure focus — is the first step toward successful treatment. One treatment option for seizures is laser ablation surgery. During the laser ablation surgery, we ablate the smallest amount of tissue possible to provide relief from seizures with minimal side effects.
How does the team identify the focus of your seizures?
First, your neurologist will analyze the pattern of symptoms that happen during your seizures; this process is called seizure semiology. The events that happen during a seizure come from specific parts of your brain, so the seizure semiology provides a map of where the seizure is going in your brain. This is the first step to identifying where your seizures may be starting.
Next, a scalp EEG – or electroencephalogram – tracks the electrical activity of the brain, and your neurologist uses this information to create a second brain map.
Then, you will undergo an MRI (magnetic resonance imaging), PET (positron emission tomography) or SPECT (single photon emission tomography) scan. The neurologist analyzes the scan results in conjunction with the EEG to further understand what is happening in your brain. Sometimes another mapping technique, an MEG (magnetoencephalogram), is also used.
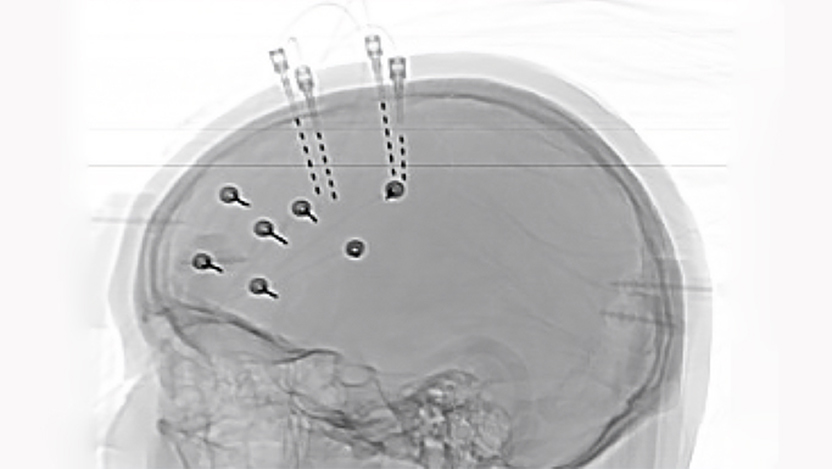
Finally, using data from all available brain maps, your neurosurgeon implants thin depth electrodes into your brain for one to two weeks. The electrodes detect the exact location or locations where the seizures start. The information gathered from the electrodes will tell your physician team exactly where to operate.
How does a laser ablation procedure treat epilepsy?
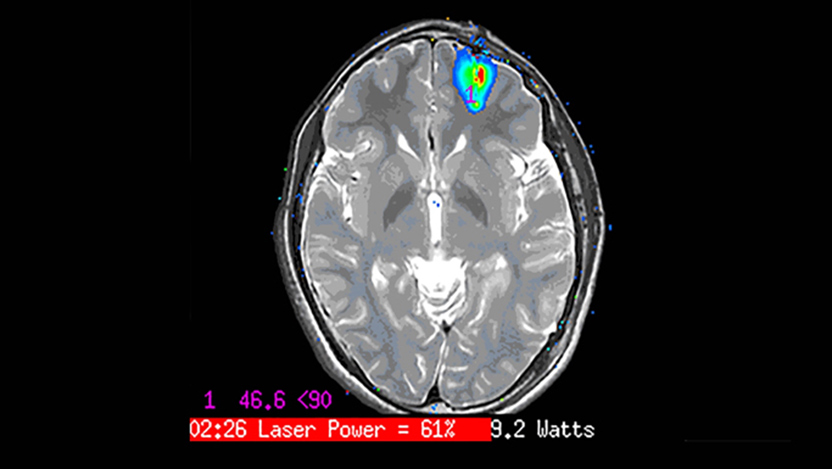
During a laser ablation procedure – also known as laser interstitial thermal therapy (LITT) – a neurosurgeon uses targeted laser technology to deliver heat to ablate, or destroy, the cells responsible for causing seizures.
To reach the impacted areas of the brain, the surgeon makes a tiny incision about the size of the barrel of a pen in the skull. They will remove your hair to have a clear view, but don’t worry – it will all grow back.
The surgeon uses a stereotactic frame or a robot in conjunction with an intraoperative CT in the operating room to see exactly where the laser should be applied, and then inserts the laser probe into your brain at the exact area of the seizure focus.
Because of the detailed mapping process performed before surgery, the neurosurgeon knows exactly where to target the ablation so that only the responsible cells are destroyed. The actual ablation is then carried out in the MRI scanner under continuous image monitoring and real-time assessment of the brain temperature. Every seven seconds the ablated tissue is assessed with a precision of 0.5 mm; critical brain structures are monitored and protected by a safety temperature limit, shutting off the laser automatically if a specific temperature is reached.
What to expect after surgery
After the laser ablation is complete, your surgical incision is closed, and you will spend one to two days in the hospital before going home. Most people get back to their normal lives within one week.
The efficacy of the laser procedure depends on the type of epilepsy and the location of the seizure focus. You will want to continue to see your neurologist to manage any symptoms.
To learn more or to make an appointment with UChicago Medicine's Level 4 Epilepsy Center, call 703-702-6222.
Peter Warnke, MD
Internationally renowned neurosurgeon Peter Warnke, MD, has performed more than 5,000 stereotactic surgeries and more than 2,000 brain tumor surgeries. Dr. Warnke provides neurosurgical care for the treatment of adults and children with movement disorders, epilepsy and brain tumors.
Learn more about Dr. Warnke
Naoum P. Issa, MD, PhD
Naoum Issa, MD, PhD, is a neurologist specializing in the treatment of epilepsy. He works closely with patients to control their seizures and is passionate about offering advanced options for epilepsy that is resistant to anti-seizure medications.
Read Dr. Issa's physician bio