Cancer cells cooperate to fight off the immune system and overcome therapy
One such mechanism is the expression of a protein called PD-1 on the surface of T cells. When bound by its ligand, PDL-1, T cells become inactivated, creating a major limit to the immune response. The ligand, PDL-1, is expressed on many cell types, and it is up-regulated following T cell activity. Cancer cells are able to hijack this method of T cell suppression by producing PD-L1 and directly turning off T cells. Although there are many pathways that inactivate T cells, the PD-1/PDL-1 mechanism is a dominant method that cancer cells use to directly disarm T cells.
Gajewski’s tenure with the Comprehensive Cancer Center
For more than two decades at the Comprehensive Cancer Center, investigator and clinician Thomas Gajewski, MD, PhD, AbbVie Foundation Professor of Cancer Immunotherapy, has been leading efforts to develop and improve immunotherapies against cancer. His work on the PD-1/PDL-1 checkpoint contributed to the development of the first trials in melanoma and, over time, the cancers being treated have expanded dramatically because the biology is similar across most solid tumor types.Gajewski's body of research is shifting the field toward a more complete understanding of tumor immune resistance mechanisms, both within the tumor, and environmental and genetic factors from the patient.There are now FDA approvals of PDL-1 and PD-1-blocking antibodies in around 15 types of cancer and, in several cancers, these antibodies, either alone or in combination, are becoming a first line of therapy. This is because when patients do respond, the responses can be very durable, and some patients appear to be cured — even when they initially have advanced disease.
“The durability of the response is very attractive,” Gajewski remarked. “But the problem is that many patients have a very limited clinical benefit, and so the big question is why doesn’t everyone have that major response.”
Gajewski maintains his drive to investigate the biology that mediates tumor cell resistance to immune destruction through a deep intellectual curiosity. His commitment to cancer immunotherapy began during his postdoctoral fellowship in Brussels, Belgium, in the lab of Dr. Thierry Boon, who is known for identifying the first tumor antigens. During his time with the Boon lab, Gajewski was awestruck by the observation that you could make a tumor cell line from a patient, and you could make a cytotoxic T cell line from that patient, and grow them up separately.
“[It’s] sort of like separating the fighting siblings and putting them on the opposite ends of the room, and then when you put them back together… the T cells would kill the tumor cells, but for some reason they didn’t when they were in the patient.” This extraordinary realization, that T cells could kill tumor cells, illuminated his path forward.
Step by step
The challenge of addressing why tumor-targeting T cells do not always work in the patient requires a methodical, step-by-step approach to ultimately “figure out the whole universe of mechanisms by which cancer can resist immune destruction,” according to Gajewski.
Therefore, Gajewski was determined to avoid just looking under the streetlight. Instead, he devised a system to capture what these mechanisms are, in an unbiased way. His strategy was to use a genome-wide CRISPR library to disrupt genes randomly throughout the entire genome of the cancer cells. This is like making gene knock-out cells, but instead of focusing on one gene, you can use CRISPR gene-editing technology to look at tens of thousands of genes within one experiment. The Gajewski lab would use these cells to pinpoint which genetic changes within the cancer cells were allowing them to defeat the immune system. They paired these CRISPR cancer cells with T cells to see which genetic mutations allowed the cancer cells to avoid T cell killing and continue to progress.
This experiment led to the discovery of a cell signaling deficiency that alters the susceptibility of cancer cells to T cell killing. A series of cancer cells that pulled ahead in this experiment had mutations in an immune pathway called the Interferon-γ signaling pathway. These data linked to recent clinical work that found this same pathway was defective in the tumors of cancer patients that were unresponsive to immunotherapy treatment.
The team was thrilled to move this clinically relevant finding into a living model system — until they hit an unexpected turn. They found that these tumors were demolished in the animal model, which was the opposite of the result they expected. In fact, the cancer cells were highly susceptible to immune killing and were wiped out even faster than the non-signaling-deficient cells. Gajewski’s team moved forward, determined to resolve this paradox between the research results and the clinical data.
Importantly, they discovered that these signaling-deficient cells did not express PDL-1, the surface molecule that works to inhibit T cells. Therefore, the T cells were easily able to attack and kill these tumor cells without resistance. After they figured out that these cells lacked PDL-1, they were no longer surprised that the tumors had been easily destroyed in an animal model. The conflict still existed that these signaling-deficient cancer cells could prosper in patients. They realized that one possibility for the discrepancy was the heterogeneous (consisting of different cells) nature of tumors in patients. They then asked, what is the impact of heterogeneity on the ability of various clones to evade immune destruction?
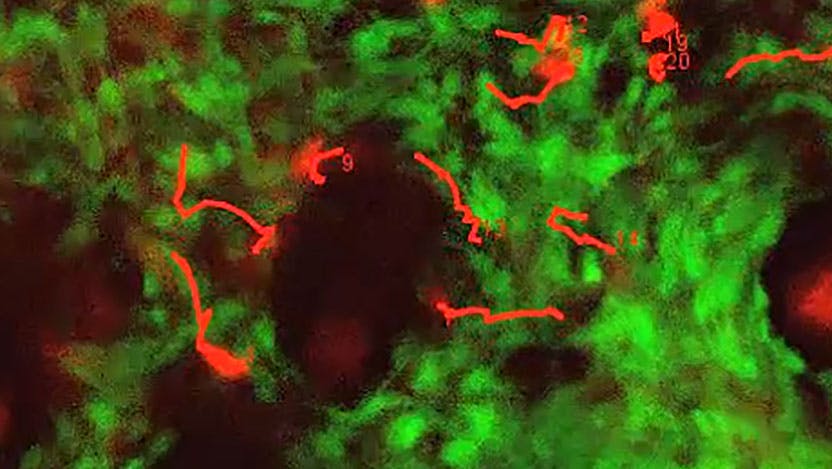
The team surged ahead, creating a model that allowed them to investigate the progression of heterogeneous tumors, by mixing cells together that were genetically different. They wanted to look at how this would impact tumor growth during and after treatment with checkpoint inhibition, in order to learn about what might be happening in non-responsive patients that had tumors with this same type of mutation.
Finally, the team got the answer to their paradox. When the two types of cancer cells were mixed together, it allowed the signaling-deficient type to evade the immune system and stay alive. Gajewski reasoned that these cells were able to overcome checkpoint inhibition and escape immune destruction due to cooperation with the cells that had a normal signaling pathway, and normal PD-L1 expression.
When these mixed tumors were treated with checkpoint inhibition, it reenacted what happened in patients. The signaling-deficient cells were able to avoid immune destruction and even outgrow their PD-L1-expressing neighbors. This is a new example of an emerging theme of “clonal cooperation” in cancer biology, which requires at least two different populations of cells that appear to help each other out, allowing for the growth of populations that would be defeated if they were on their own. “These data suggested, for the first time, that clonal cooperation among subpopulations of tumor cells might be important for resistance to immunotherapy,” said Gajewski.
Gajewski’s recent discovery, which was published in Nature Communications1, has important implications for the clinical care of cancer patients. He said, “The involvement of tumor heterogeneity in promoting clonal cooperation as a mechanism of tumor resistance to checkpoint inhibition therapy suggests that if we treat patients earlier in their disease course — before the tumor has continued to accumulate mutations and become more heterogeneous — the clinical outcomes could be better and tumor resistance may be less likely.”
Accordingly, there are currently multiple ongoing clinical studies with neoadjuvant immunotherapy, which give checkpoint inhibition antibodies very early in the course of a patient’s disease, even when they first present and before their surgery. It is possible that if treated before metastasis, the immune cells will have a better chance of tumor destruction. Gajewski’s idea is to “treat early, hit ’em hard, and try to kill the vast majority of tumor cells before they have years to develop heterogeneity and resistance.”
Future directions
To fully appreciate how tumors evade immune destruction during immunotherapy treatment, Gajewski believes that researchers must also go beyond focusing on these changes within the tumor, which are critical, but only a part of the picture. Another goal of his is to zoom out from the cancer to the whole patient, and that’s where his team found that there are environmental factors that impact the host immune response2.
“For example, there are certain gut microbes that strengthen the immune response and we now know there are other gut microbes that hold back the immune response,” he explained. This raises the possibility of modulating the microbiota in order to influence the response to immunotherapies.
Another consideration that the Gajewski lab is pursuing is a complete understanding of germline genetics, or inherited genes. They have identified germline variants which are functionally relevant for anti-tumor immunity. Understanding the impact of inherited genetics has the potential to personalize immunotherapy approaches.
Gajewski's body of research is shifting the field toward a more complete understanding of tumor immune resistance mechanisms, both within the tumor, and environmental and genetic factors from the patient. This complete picture can help guide future improvements of immunotherapies in the clinic.
References:
1

Thomas F. Gajewski, MD, PhD
Thomas Gajewski, MD, PhD, investigates and develops new treatments for patients with melanoma. He also leads development of immune-based therapies for other cancers, using new laboratory data on how the immune system is regulated to develop novel clinical trials.
Read Dr. Gajewski's physician profile